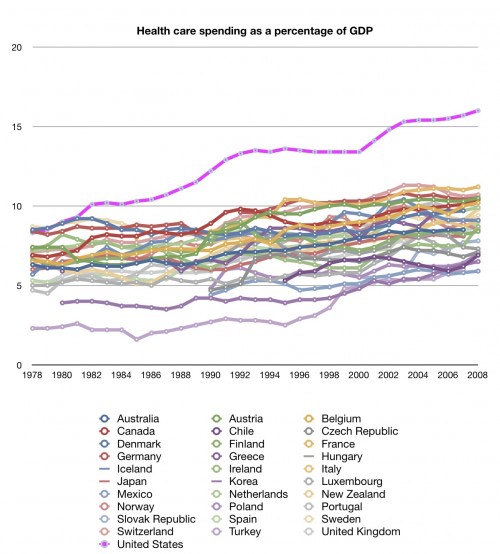
The US health system has many puzzles. Here’s one: why did US spending relative to GDP diverge from that of other wealthy nations around 1980? Check it out in this graph by Aaron, which we’ve posted many times, including earlier today:
We’ve pondered this and related 1980s trivia before and not come up with a good explanation. In the comments, Donna Kinney offers a new idea.
The change in the 80′s was the introduction of third-party payment and low or no deductibles in early managed care plans. Prior to tgrowing market penetration, patients paid out of pocket for most services and were reimbursed by insurers. […] Third party payment in Medicare also started in the early 80′s, freeing Medicare beneficiaries from up-front spending and claims filing.
Third-party payment decreased the out-of-pocket cost for patients, decreasing the percieved price of care and driving demand and utilization up. Third-party payment increased the operating cost of providers and payers because of the claims handling costs on both sides of the transaction and also because the payers had to add new procedures and programs design to control utilization growth. Those utilization control programs might have limited cost growth during the 90′s but they had also been responsible for some of the cost growth during the ’80s as both payers and providers added new administrative burden.
It sounds intriguing, but it leads to some obvious questions:
- What publications document the notion that we can hang the spending divergence on third-party payment?
- Other nations have third-party payment. That being the case, why is the US pulling away?
One possibility is that third-party payment is a necessary but not sufficient condition for such explosive spending growth. One also needs the third parties to have little to no ability to exert utilization control. When they can exert that control, spending growth diminishes. I’m tempted to point to the 1990s as evidence of this, but we know that’s as much a GDP growth story as a health care spending story.