Fully developed posts on syringe exchange programs (SEPs) are here and here. A couple more are forthcoming. Here are the notes I took as I read the literature in this area. This is Part III. Part I is here. Part II is here.
(1) Head of ONDCP Promotes Needle Exchange Programs (Partnership for Drug-Free Kids, 2015)
- “Needle-exchange programs are effective tools to fight the spread of infectious disease and steer heroin users into treatment, according to Michael Botticelli, Director of the Office of National Drug Control Policy. ‘They’ve been demonstrated to reduce not only infectious disease but also create an opportunity for people to get the care and provide a transition into treatment for people in the community,’ he said […] at an event sponsored by the Northern Kentucky Chamber of Commerce.”
- “Kentucky Governor Steve Beshear recently signed a bill into law that will allow local health departments to set up needle exchanges after obtaining approval from local governments. In Indiana, Governor Mike Pence declared a state of emergency in response to a growing number of HIV cases linked to intravenous use of the painkiller Opana. He authorized a short-term program in one county to allow people to exchange used needles for sterile ones, to reduce the risk of contaminated needles being shared. There are about 200 needle-exchange programs in 33 states and the District of Columbia, according to the North American Syringe Exchange Network.”
(2) Syringe Sharing and HIV Incidence Among Injection Drug Users and Increased Access to Sterile Syringes, by Thomas Kerr et al. (American Journal of Public Health, 2010)
- “[W]e examined syringe borrowing, syringe lending, and HIV incidence among a prospective cohort of 1228 injection drug users in Vancouver, British Columbia. Results. […] In multivariate analyses, the period following the change in SEP policy was independently associated with a greater than 40% reduction in syringe borrowing (adjusted odds ratio [AOR]=0.57; 95% confidence interval [CI]=0.49, 0.65) and lending (AOR=0.52; 95% CI=0.45, 0.60), as well as declining HIV incidence (adjusted hazard ratio=0.13; 95% CI=0.06, 0.31).”
- “Previous evaluations of SEPs have demonstrated that these programs are associated with reductions in syringe sharing and HIV incidence [Wodak] as well as increased rates of entry into addiction treatment programs [Heimer, Strathdee] Further, previous evaluations have found that SEPs do not increase drug use, crime, or discarded syringes [Watters].”
(3) Evidence for the effectiveness of sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus transmission among injecting drug users: a review of reviews, by Norah Palmateer et al. (Addiction, 2010)
- “Three core and two supplementary reviews of injecting equipment interventions were identified. According to the proposed framework, this study found (a) insufficient evidence to conclude that any of the interventions are effective in preventing HCV transmission; (b) tentative evidence to support the effectiveness of NSP [needle and syringe programs] in preventing HIV transmission; (c) sufficient evidence to support the effectiveness of NSP (and tentative evidence of an additional impact of pharmacy NSP) in reducing self-reported IRB [injecting risk behavior]; and (d) little to no evidence on vending machines, outreach or providing other injecting equipment in relation to any of the outcomes.”
- [As discussed in Wodak and Cooney, below, some studies done in the presence of legal access to syringes at pharmacies find negative or null results of SEPs (or NSPs).]
(4) Do Needle Syringe Programs Reduce HIV Infection Among Injecting Drug Users: A Comprehensive Review of the International Evidence, by Alex Wodak and Annie Cooney (Substance Use & Misuse, 2006; referenced in (2), above and in Part I (1)). See also the WHO report by the same authors.
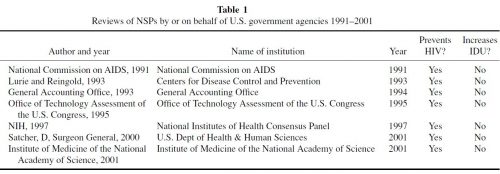
- “The principal finding of this review was that there is compelling evidence of effectiveness, safety, and cost-effectiveness, consistent with seven previous reviews conducted by or on behalf of U.S. government agencies.”
- “By the beginning of the 1990s, evidence of the effectiveness and safety of NSPs in reducing HIV spread among IDUs was already compelling and well summarized in seven previous reviews conducted by or on behalf of U.S. government agencies (Table 1). The failure of these reviews to influence the policymaking process in the United States has to be considered from the perspective of an unusual national drug policy sustained over many decades (McAllister, 2000; MacCoun and Reuter, 2001; McCoy, 2003). Authorities, especially in developing and transitional countries, have often resisted implementation of NSPs lest any support for effective harm reduction strategies might be considered to undermine their entrenched commitment to global drug prohibition. […] Adoption of NSPs in the United States has been late and implementation slow because of explicit rejection of harm reduction and strong support for a zero tolerance approach to drugs.”
- “Forty-five studies dating from 1989 to 2002 were identified with NSP implementation as an intervention and HIV seroconversion, HIV seroprevalence, or HIV risk behaviors among IDUs examined as outcome variables. […] Six of ten studies that evaluated HIV seroconversion or seropositivity as outcomes found that NSP use was protective. […] HIV risk behavior outcomes were examined in 33 studies. […] Most focused on syringe sharing, borrowing, lending, or reuse (23 positive).”
- “Conclusions: 1. There is compelling evidence that increasing the availability, accessibility, and both the awareness of the imperative to avoid HIV and utilization of sterile injecting equipment by IDUs reduces HIV infection substantially. […] Measured against any objective standards, the evidence to support the effectiveness of NSPs in substantially reducing HIV must be regarded as overwhelming. 2. There is no convincing evidence of any major unintended negative consequences. Specifically and after almost two decades of extensive research, there is still no persuasive evidence that NSPs increase the initiation, duration, or frequency of illicit drug use or drug injecting. 3. NSPs are cost-effective. It is more difficult to generalize from studies of cost-effectiveness of NSPs in one country to other similar countries, let alone from developed countries to resource-poor settings. However, a number of careful studies in several developed countries and some transitional countries have demonstrated convincingly that NSPs are cost-effective. 4. NSPs have additional and worthwhile benefits apart from reducing HIV infection among IDUs. There is reasonable evidence that NSPs can increase recruitment into drug user treatment and possibly also into primary health care.”