Fully developed posts on syringe exchange programs (SEPs) are here and here. A couple more are forthcoming. Here are the notes I took as I read the literature in this area. This is Part I. Part II is here. Part III is here.
(1) Lessons from Indiana: the case for broader implementation of syringe exchange programs, by Monica Ruiz, Sean Allen, and Allison O’Rourke (Harvard Health Policy Review, 2015)
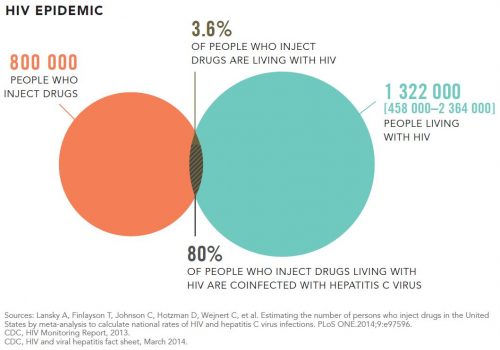
- The first HIV outbreak in the US in three decades occurred in 2015 in rural Indiana. The source of the spread: injection drug use (IDU).
- Syringe exchange programs, which are effective in reducing the spread of blood borne disease, are restricted by policy at federal, state, and local levels.
- The first SEPs in the U.S. opened in the 1980s. Today there are 133. “Since the implementation of SEPs, IDU-attributable HIV incidence in the US has declined by approximately 80%; this is the only category of adult HIV infection to show declines of this magnitude.”
- Most laws governing injection equipment are “rooted in the perception of addiction as a criminal rather than public health issue.” Over the years, states and municipalities passed laws that restricted the sale and distribution of sterile injection equipment, though some have been reformed in response to public health crises.
- From 1988 to 2009, a federal law banned the use of federal funds for SEPs. The ban was lifted between 2009 and 2012, during which time three SEPs received federal funding. The ban remains in effect today.
- Until 2007, Washington DC is the only U.S. city prohibited by Congress to use municipal funds for SEPs.
- “Bowen [argues] that US drug policy [] is ‘a charged issue, largely driven by values and morals, instead of logic, economics, and principles of public health.’ This irrationality extends to community-level policy decisions, manifested through ‘not in my backyard’ ideologies that marginalize already disenfranchised groups, such as PWID, the homeless, and the mentally ill.”
- “In Baltimore and Philadelphia, research guided policy discussions and helped change policymakers’ and constituents’ conceptualizations about substance use and the utility of SEPs. In DC, the unwillingness of Congressional SEP opponents to consider research evidence proved to be a significant impediment. Several stakeholders described Congress as an ‘evidence-free zone’ where SEP opponents misinterpreted research findings or took evidence out of context to support their opinions. One person commented, ‘…Whether you quoted from scientific journals…and…statistical evidence, from what was happening across the United States, none of it mattered.'”
- “Research evidence overwhelmingly demonstrates that SEPs successfully reduce HIV incidence as well as injection-related practices that increase HIV and HCV risk [Ksobiech, Hurley, Palmateer, Tilson, Wodak,* Hagan [also examines hepatitis B], Kaplan]. Data from the earliest SEPs are the most impressive: in Tacoma, SEPs were associated with an over 80% reduction in the incidence of hepatitis B and C infections. Similarly, SEPs were associated with a 33% reduction in HIV infection in New Haven, CT, and a 70% reduction in New York, NY.”
- “Numerous modeling studies show that widespread clean syringe access results in substantial financial savings compared to costs associated with lifetime HIV treatment [Lurie, Holtgrave, Laufner]. Lurie and Drucker* estimated that between 4,394 (15% incidence reduction) and 9,666 (33% incidence reduction) HIV infections could be averted as a result of implementing SEPs nationally, resulting in a $244 to $538 million (in 1997 USD) costs savings to the US healthcare system. Extrapolating to 2015 USD, the savings are approximately $361 to $796.5 million. Our research found similarly impressive cost-savings. In the two years following the DC Ban’s removal, we estimated 120 averted HIV infections.* The Centers for Disease Control and Prevention (CDC) estimated the average lifetime cost of treating HIV at $380,000 USD per person. Subtracting SEP operational costs, averting 120 cases of HIV translates to an approximate cost savings of $44.3 million USD. Given that the clinical care (including prescriptions) of many HIV-positive DC residents is covered by the city’s publicly funded health plan, costs saved in treatment are direct savings to DC taxpayers.”
- “Given recent law enforcement crackdowns on prescription drug misuse, the transition from prescription opiates to cheaper, more easily accessible illicit drugs is inevitable. A recent Substance Abuse and Mental Health Services Administration (SAMHSA) report found that the number of people ages 12 and older who reported using heroin in the past year rose from 373,000 in 2007 to 681,000 in 2013, an 83% increase.”
- “Acting on the Executive Order 15-05 issued by Governor Mike Pence, State Health Department officials were able to act quickly to establish a SEP in Scott County in less than 2 months since the initial news of the outbreak, overriding existing legislation declaring such programs to be illegal in the state. Through this Executive Order, Governor Pence showed that he could suspend his own views about needle exchange (he has previously voiced opposition to SEPs), focus on the research evidence supporting this intervention, and respond quickly to the public health need that mandated it.” The Indiana legislature also acted.
(2) CDC:
- 13 percent and five percent of HIV infections in U.S. women and men, respectively, are attributed to injection drug use (2014 data).
(3) Global estimates of prevalence of HCV infection among injecting drug users, by Carmen Aceijas and Tim Rhodes
We identified 10 estimates of HCV antibody prevalence among IDUs in the USA []. The lowest estimate was in Baltimore in 2002 (8% of 183 IDUs), while other estimates ranged from 28 to 88% []; the latter from Albuquerque (New Mexico) in a study of 516 IDUs recruited through treatment facilities and via a community survey in 1996. An estimate of 83% was reported among 229 IDUs, recruited in similar settings in Las Cruces (also New Mexico) []. Estimates from New York show 71% of 89 IDUs recruited in treatment services and tested in 2001 and 61% of 314 IDUs participating in a survey between 2001 and 2003, to be HCV positive.
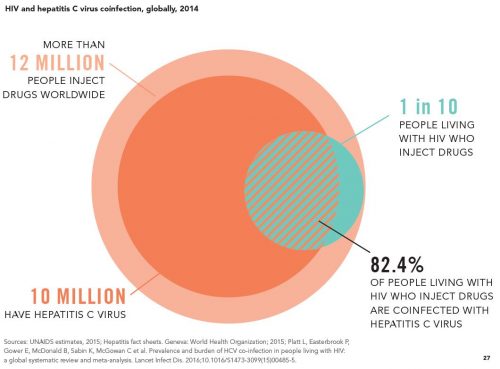
(4) Do no harm – Health, human rights and people who use drugs (UN AIDS, 2016)
- “Needle–syringe programmes reduce the probability of transmission of HIV and other bloodborne diseases by lowering the rates of sharing of injecting equipment among people who inject drugs [Hunt, Gibson].”
- “Ten years of needle–syringe programming in Australia reduced the number of cases of HIV by up to 70% and reduced the number of cases of hepatitis C by up to 43%. […] [E]ach dollar spent on Australia’s needle–syringe programme between 2000 and 2010 has an estimated lifetime return on investment of US$ 1.30–5.50 in averted health-care costs [Kwon].”
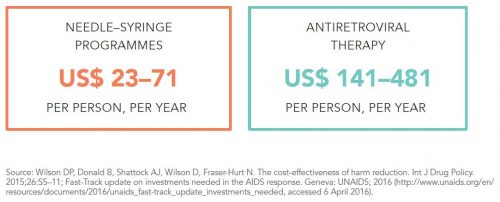
- “Costing US$ 23–71 per person per year, needle–syringe programmes are relatively inexpensive to implement and are much more affordable than the lifetime health-care costs required to treat a person living with HIV [Wilson]. Cost-effectiveness is even higher if we consider the combined reduction of HIV and hepatitis C infections [Wright].”
- “The preamble of the Single Convention on Narcotic Drugs describes dependence on narcotic drugs as a ‘serious evil for the individual’ and ‘fraught with social and economic danger to mankind’. Community advocacy organizations have denounced such language as emblematic of the demonization of people who use drugs and the stigma and discrimination they face in their daily lives [Albers].”
- “Judgemental feelings among health-care providers have been linked to lower-quality health care and lower health outcomes [Skinner, Treloar]. Nearly one quarter of people who use drugs surveyed in the United States reported they had been prevented from obtaining medical care because of their drug use, and one third said they had been denied housing because other people knew about their drug use [Ahern].”
- “In the United States, federal law calls for people with drug-related convictions, including for personal possession and use, to be denied housing assistance, nutritional support, cash transfers, and grants and loans for higher education [Levi]. Individuals coming out of prison for drug related crimes are thus denied social support services at a time when they may need it the most, increasing the likelihood that they will drop out of drug dependence treatment, struggle to find employment and suffer from food insecurity [The Sentencing Project]. Former prisoners who live in states that fully enforce the federal ban on nutritional support are more likely to report having gone an entire day without eating than those who live in states that do not enforce the ban. Furthermore, a study showed that people who did not eat for an entire day were more likely to engage in risky behaviour, such as using alcohol, heroin or cocaine before sex or exchanging sex for money [Wang].”
- “The Consolidated Appropriations Act of 2016 gives states and local communities the opportunity to use federal funds to support certain components of needle-syringe programmes.” Though federal funds can used to support aspects of these programs, “they cannot be used to purchase sterile needles or syringes for illegal drug injection.”