Fully developed posts on syringe exchange programs (SEPs) are here and here. A couple more are forthcoming. Here are the notes I took as I read the literature in this area. This is Part II. Part I is here. Part III is here.
(0) Impact Evaluation of a Policy Intervention for HIV Prevention in Washington, DC, by Monica Ruiz, Allison O’Rourke, and Sean Allen (AIDS Behav, 2016; See Part I, item (1))
- “The District of Columbia (DC) is in the midst of a significant HIV/AIDS epidemic. According to epidemiological data from the end of 2011, approximately 2.4% of DC residents over the age of 12 years are living with HIV/AIDS. Injection drug use (IDU) accounts for 14.2% of the living cases of HIV/AIDS in the District [DC Dept. of Health].”
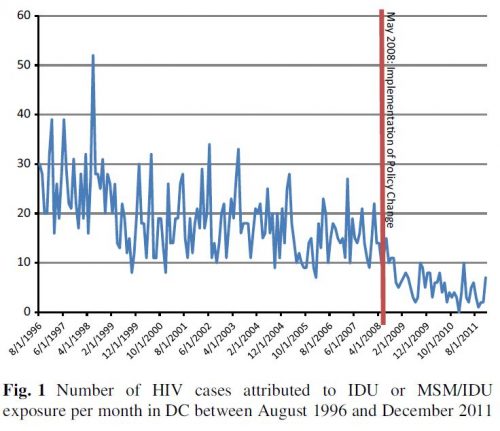
- In May 2008, a ban on use of DC municipal funds for SEPs was lifted. “Then-Mayor Adrian Fenty allocated $650,000 to the DC Department of Health to create the DC NEX, a program supporting several CBOs [community-based organizations] in delivering a minimum harm reduction package that includes syringe exchange, provision of condoms, referrals to HIV testing and addiction treatment, and harm reduction information [Greenberg].” This study examined the impact of these changes on injection drug use-caused HIV cases.
- “Our modeling of the forecasted versus actual epidemic curves shows that, as a result of the removal of the DC Ban, there was a 70% decrease in the number of newly diagnosed HIV cases where reported mode of transmission was IDU.”
(1) Quantifying Syringe Exchange Program Operational Space in the District of Columbia, by Sean Allen, Monica Ruiz, and Jeff Jones (AIDS and Behavior, 2016)
- “In the United States (US), an estimated 2.6% (approximately 6,612,488 persons) of the population [above 12 years of age] has ever injected drugs.”
- “In the United States, IDU [injection drug use] is the most common route of HCV [hepatitis C virus] transmission.”
- According to one estimate, 90% of DC injection drug users have hepatitis C.
- “SEPs may also provide health education on topics that are relevant to PWID, such as how to engage in safer injection practices (e.g., not sharing injection equipment, how to sterilize syringes, etc.) and how to prevent overdose [avert.org].”
- “The [1914] Harrison Act [] made the possession of injection equipment illegal without a prescription.” A significant limitation today is the prohibition of use of federal funds for distribution of injection equipment to injection drug users. “The implementation of buffer zone policies has also produced significant barriers to SEP operations.”
- “In 2000 DC government passed the 1000 Foot Rule (§48–1121), prohibiting the distribution of ‘any needle or syringe for the hypodermic injection of any illegal drug in any area of the District of Columbia which is within 1000 feet of a public or private elementary or secondary school (including a public charter school).'”
- “The total square mileage of the potential SEP operational space the 1000 Foot Rule caused to be ineligible for SEP activities held approximately constant over the study period, ranging from 24.30 to 25.83 square miles (50.57–53.76 % of the total area of DC).”
(2) Legal space for syringe exchange programs in hot spots of injection drug use-related crime, by Sean Allen, Monica Ruiz, Jeff Jones, and Monique Turner (Harm Reduction Journal, 2016)
- We examined the effects of the 1000 Foot Rule on SEP operational space in injection drug use (IDU)-related crime (i.e., heroin possession or distribution) hot spots from 2000 to 2010.”
- “When overlaying the land space associated with IDU-related crime hot spots on the maps of school boundaries per the 1000-ft buffer zone stipulation, we found that the majority of land space in these locations was ineligible for legal SEP operations. More specifically, the ineligible space in the identified hot spots in each academic year ranged from 51.93 to 88.29 % of the total hot spot area.”
(3) Assessing Syringe Exchange Program Access among Persons Who Inject Drugs (PWID) in the District of Columbia, by Sean Allen, Monica Ruiz, Jeff Jones (Journal of Urban Health, 2016)
- “The results of this research suggest that the distance DC PWID traveled to access SEP services remained relatively constant (approximately 2.75 mi) from 2003 to 2008, but increased to just over 4 mi in 2010.”
(4) An opportunity lost: HIV infections associated with lack of a national needle-exchange programme in the USA, by Peter Lurie and Ernest Drucker (Lancet, 1997; See Part I, item (1))
- “In Amsterdam, a needle-exchange programme opened as early as 1984, in an effort to reduce the transmission of blood-borne infections such as hepatitis B. Thus, when evidence on the efficacy of such programmes began to accumulate, most countries in western Europe, as well as in Australia, New Zealand, and Canada, were able to move rapidly to provide sterile syringes to IDUs [injection drug users] through a combination of needle-exchange programmes and increased availability of sterile injection equipment through pharmacies. By contrast, in the USA, opposition to needle-exchange programmes arose from some drug-treatment providers, ethnic minority communities, law-enforcement officials, politicians, local business people, and residents. These groups asserted that programmes would lead to increased drug use and would also divert public funds from already under-funded drug-treatment facilities.”
- “Six government-sponsored reviews of needle-exchange programmes [Normand, Lurie, GAO, National Commission, Office of Technology Assessment, one unavailable on the internet] concluded that such programmes reduce the incidence of HIV infection among IDUs and do not lead to an increase in rates of drug use.”
- After reviewing the evidence, in 1993, the CDC recommended that the ban on Federal funding of exchange programs be lifted.”
(5) Syringe exchange in the United States: a national level economic evaluation of hypothetical increases in investment, by Trang Quynh Nguyen et al. (AIDS Behav, 2014)
- “HIV infections cause significant human suffering and exact substantial financial costs, with each infection in the United States estimated to result in a loss of between 9 and 21.1 years of life [Harrison], between 5.33 and 6.433 quality adjusted life years [Holtgrave, Hutchison], and $379,668 (2010 dollars) in lifetime treatment costs [CDC]. The sharing of drug injection equipment is the second-most common route of HIV transmission—approximately 9.4% of new HIV infections in the United States in 2009 occurred among persons who injected drugs (PWID) and 2.7% occurred among men who had sex with men and injected drugs (MSM/PWID) [Prejean].”
- “Access to sterile needles and syringes (herein referred to as ‘‘syringes’’) is a proven approach for reducing HIV transmission enumerated in the 2010 [and 2015] National HIV/AIDS Strategy for the United States. The evidence in favor of needle/syringe exchange programs (NSP) is well-documented, with economic evaluations repeatedly showing that NSPs are cost-effective and cost-saving for the prevention of HIV [Gold, Jacobs, Laufer, Cabases, Kumaranayake]. The 2012 US President’s Emergency Plan for AIDS Relief (PEPFAR) Blueprint envisions an AIDS-free generation within our lifetime, calling for ‘‘smart investments based on sound science’’, and establishing NSPs as one of the three central elements of the PEPFAR comprehensive prevention package for PWID, in addition to community-based outreach programs and drug treatment.”
- “Many NSPs provide additional services such as referrals to drug treatment programs, HIV testing and counseling, and condom distribution [Des Jarlais].”
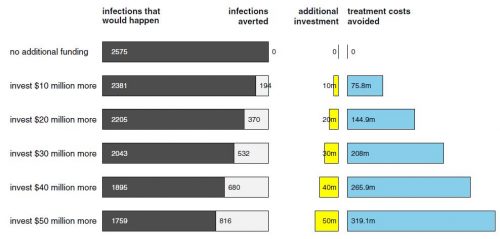
- “With an annual $10 to $50 million funding increase [for SEPs], 194–816 HIV infections would be averted (cost per infection averted $51,601–$61,302). Contrasted with HIV treatment cost savings alone, the rate of financial return on investment would be 7.58–6.38. Main and sensitivity analyses strongly suggest that it would be cost-saving for the US to invest in syringe exchange expansion.”
(6) Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors, by Holly Hagan et al. (Journal of Substance Abuse Treatment, 2000)
- “The association between needle exchange, change in drug use frequency and enrollment and retention in methadone drug treatment was studied in a cohort of Seattle injection drug users (IDUs). Participants included IDUs classified according to whether they had used a needle exchange by study enrollment and during the 12-month follow-up period. The relative risk (RR) and the adjusted RR (ARR) were estimated as measures of the association. It was found that IDUs who had formerly been exchange users were more likely than never-exchangers to report a substantial (> or= 75%) reduction in injection (ARR = 2.85, 95% confidence limit [CL] 1.47-5.51), to stop injecting altogether (ARR = 3.5, 95% CL 2.1-5.9), and to remain in drug treatment. New users of the exchange were five times more likely to enter drug treatment than never-exchangers.”
- “In this study, there was no indication that needle-exchange use was associated with increasing drug use. Indeed, IDUs who were former users of the exchange were more likely than never-users to report substantial reductions in drug use or stopping injection altogether. Our analysis also suggested that among heroin injectors, needle-exchange participation was wholly compatible with the goals of drug treatment. Compared to those who had never used an exchange, new exchange users were five times more likely to enter methadone treatment and ex-exchangers were 60% more likely to remain in methadone treatment over the 1-year study period.”
- “[T]here are a number of studies showing that the net effect of an exchange might be to reduce drug use, particularly through recruitment to drug treatment [Brooner et al., 1998; Guydish et al., 1993; Hagan et al., 1993; Hartgers et al., 1989].”
- Some SEPs have operated illegally.