This is a TIE-U post associated with Jonathan Kolstad’s The Economics of Health Care and Policy (Penn’s HCMG 903-001, Spring 2012). For other posts in this series, see the course intro.
What’s the central issue in health economics? Tom McGuire’s answer in the first sentence of his Physician Agency (ungated pdf) [1] is that it is physician behavior. Though McGuire covers many related topics, one of the main areas of exploration in his paper is physician (or supplier) induced demand (SID).
Historically, within health economics SID has been a contentious and controversial topic. Perhaps that’s because it rejects the canonical independence of supply and demand schedules and because it has been associated with possibly pejorative notions of wasteful over-provision of marginally beneficial (or nonbeneficial) care. I blogged on these aspects of SID yesterday.
The consternation over SID may be less common outside of health economics. McGuire writes that,
The literature outside of economics is without soul searching about whether physicians influence demand. It is nearly universally considered obvious that of course they do. The concern in this literature is usually with identifying the factors, such as socioeconomic status of patients, that lead physicians to direct patients to different courses of therapy.
Within health economics the evidence cited by McGuire at the time of his paper (year 2000) was somewhat mixed, but he concludes that,
Adding up the evidence, on obstetricians doing more C-sections, surgeons doing more bypass operations, physicians referring more frequently to their own labs, and other studies, makes a convincing case that doctors can influence quantity and sometimes do so for their own purposes.
What’s meant by “for their own purposes”? Many point to financial incentives. McGuire quotes Mark Pauly [2],
“Other things equal, physicians would rather tell the truth, but they would be willing to surrender some accuracy for some amount of money income.” Once that tradeoff is admitted, it is hard to avoid the conclusion that the physician will be inducing some demand.
Though I don’t think it is necessary to imply physicians are lying to their patients, recent evidence also supports the very conclusion McGuire reached, that physicians induce some demand, consistent with their financial interests. You can click back to my post about a randomized experiment that reaches that conclusion and links to other work. More recently, Christel van Dijk and colleagues found that in the Netherlands,
introduction of fee-for-service for socially insured consumers led to a higher increase in physician-initiated utilisation. […] Differences in the trend in physician-initiated utilisation point to an effect of supplier-induced demand.
(Their paper also includes an up-to-date literature review of SID.)
However, physicians might induce demand even in the absence of financial incentives to do so. This can occur when patients are not fully informed and defer to their physicians for treatment decisions. John Wennberg describes the stereotypical physician-patient model in Tracking Medicine (highly recommended, by the way),
The patient, as a layman, does not know what he or she truly needs; it is the physician who knows the nature of the patient’s illness and can select the right treatment. For these reasons, many social scientists thought it was rational for patients to do something they would not dream of doing in most markets—that is, to delegate decision making to the seller of services, the physician, who by virtue of his special knowledge and skill, could act as their “rational agent” in health care purchasing decisions.
This, as Wennberg goes on to illustrate, is completely wrong. Evidence shows that physicians cannot act as perfect agents for patients. This comports with common sense. The nature and brevity of typical physician-patient interactions suggests that it is unlikely the physician can divine the quantity and type of care the patient would elect if fully informed.
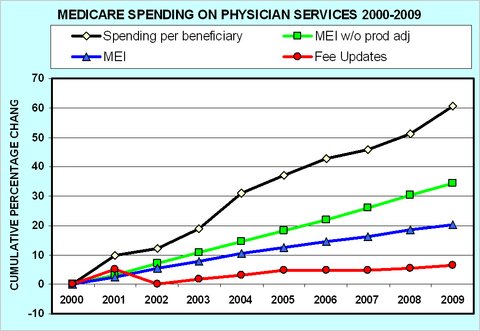
In large part, concern over physician behavior and what it means for Medicare spending is what gives rise to the doc fix debate. There a key issue is that, despite relatively modest increases in Medicare fees for doctors, per beneficiary physician spending by the program has gone up dramatically, as illustrated in the following figure by Uwe Reinhardt. (More about it here.)
It’s not a big leap to hypothesize that something about physician behavior is altering utilization patterns and driving spending up at a rate well beyond that of unit prices. A counter-hypothesis is that patients are to blame. Though (natural, un-induced) patient demand may play a role, in this population it is not credible to me that it is the only or even the most important factor.
Naturally, problems with Medicare spending motivate the search for payment systems that provide incentives for more efficient provision of care, as articulated recently on the Health Affairs blog by Michael Chernew, Darius Lakdawalla, and Dana Goldman. This is not unique to public programs. Private insurers are also seeking ways to shape provider behavior through innovations in contracting and financial incentives.
Whether or not you agree with McGuire that physician behavior is the central issue in health economics, it is central to health policy and health insurance.
References
[1] McGuire, T.G. (2000) “Physician Agency,” Chapter 9 in Handbook of Health Economics, Eds. A.J. Culyer and J.P. Newhouse, Amsterdam: North-Holland.
[2] Pauly, M.V. (1980), Doctors and Their Workshops: Economic Models of Physician Behavior (University of Chicago Press, Chicago).