The Cancer Journal is my story about being a cancer patient during the COVID-19 epidemic. In the last week, my cancer care halted because the pandemic is breaking Ontario’s health care system.
I’ll start with an update about my case. Since my radiation treatment ended in September, I’ve gotten two scans to determine whether the treatment actually worked. The initial computerized tomography (CT) scan showed that there were still significant masses at the sites of my tumour and its metastases. A follow-up positron emission tomography (PET) scan showed that these masses glowed in the image, a result consistent with them retaining living cancer cells. This was an unwelcome finding, to say the least.
I can’t get any more radiation, so I was referred to a surgeon. The surgeon, interestingly, was not impressed by the PET scan result, which he believes could be a false positive. He explained that those areas might be glowing because badly injured tissue does that. Or it might be cancer. So we need to biopsy these maybe-tumours and find out. This will not be a needle biopsy in an office, but rather a surgical procedure under anesthesia. And before the biopsy, I will need to get another CT scan, this time with radioactive contrast.
Of diagnostic procedures and their uncertainties, there is no end.
I had the CT scan last Thursday. I’ve read the radiologist’s report (and so far as I know, my surgeon hasn’t, so I may have misread it). The report’s notable finding was that an ulcer is forming at the site of my primary tumour. This is frightening, although again, for all I know, badly damaged yet not cancerous tissue might nevertheless ulcerate. Still, at least the presence of the ulcer explains my experience of continued and, in fact, growing throat pain at the site of the primary tumour. All this will, I hope, be clarified by my biopsy, which according to my surgeon’s administrator, is going to be scheduled for next week.
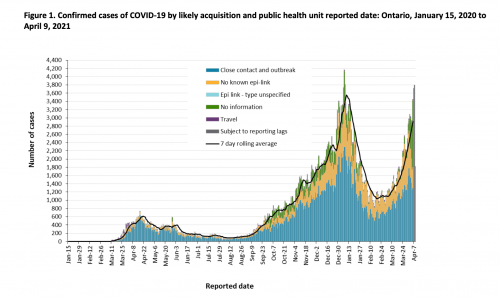
Or is it? Because now we return to the larger story of the pandemic. On Thursday, April 8, Ontario began its third shut down in response to a third wave of the epidemic. As you can see from the graph, the counts of COVID-19 cases are rapidly approaching their highest levels.
Why are there so many cases in Ontario? First, Canada is several weeks behind the US in vaccination (see this great graph by @TrevorTombe).
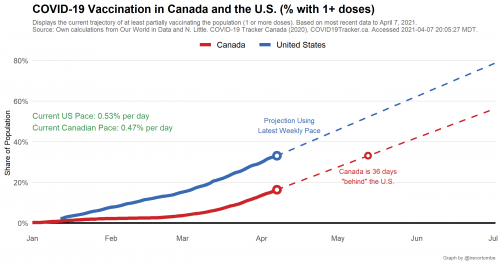
As of this morning, only 18.5% of Canadians have received at least one dose. I am not one of them, nor do I have a scheduled visit. In Ontario, you register online to be vaccinated and then wait for them to contact you. My phone hasn’t rung.
Why are fewer Canadians vaccinated? I see no evidence that vaccine hesitancy is greater than in the US. My impression is that, in general, Canadians have been more compliant with public health warnings than Americans. According to Tracey Lindeman, we negotiated a bad deal with the manufacturers.
Without much domestic manufacturing capacity to speak of, Canada had to sign advance-purchase deals with international vaccine companies. The country hedged its bet by mostly going with companies funded by Operation Warp Speed, and so far its strategy has been to overbuy doses in the hopes of securing enough to vaccinate all of its citizens. A mounting critique, however, is that perhaps Canada should have been more specific than “first quarter of 2021” in terms of arranging vaccine-delivery timing. [Toronto Globe & Mail health columnist André] Picard said that Canada, by not giving manufacturers a specific week, or even day, allowed them to push delivery until the outer limit of the quarter.
So why have the Pharma companies placed us at the end of the line for deliveries? Quoting a retired Pharma executive, Lindeman says that
long-standing Canadian policies in three areas [have been] particularly antagonistic to vaccine makers, especially multinationals: patents, prices, and procurement.
Perhaps so, but you could see this another way. Unlike the US, Canadians have bargained hard with the Pharma multinationals to get essential medications at reasonable prices. And now… this is their payback.
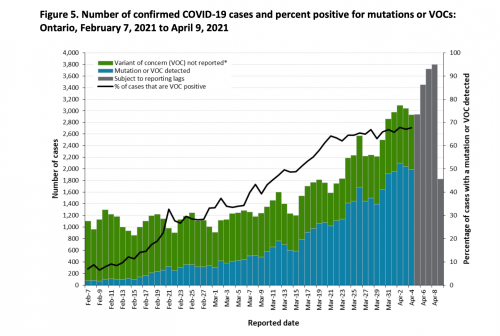
Another reason why cases have risen is that coronavirus is evolving, and at least some of the new variants have a substantially higher transmission rate than the earlier coronavirus. The faster spreading new variants will displace the older variants among new cases, and, everything else being equal, accelerate the growth in cases. As you can see in the following graph, the variant viruses have spread rapidly and now comprise 70% of new cases.
The upshot of the wave of cases is that the number of COVID-19 cases in Ontario hospitals is growing, as you can see from this graph, which I found in @thevivafrei’s Twitter feed.

Unfortunately, I can’t find a data series that expresses these case counts as a percentage of the province’s total bed or ICU capacity. My spouse participates in daily briefings about hospital capacity, and what she hears from the provincial Ministry of Health is that in many hospitals, both acute and critical care beds are at greater than 100% capacity. That means that all the standard beds are filled and patients are being cared for on gurneys. See my earlier post on ‘hallway medicine.’
If so, this is a dangerous situation. During this pandemic wave, the rate of COVID-19 deaths seems to be lower than during previous waves, possibly because the patients are younger this time. Nevertheless, people in ICUs are there for a reason: they are more likely to die if they are less closely monitored and receive less aggressive care. Unfortunately, cases requiring hospitalization are proliferating, and available beds are not. If the overcrowding gets worse, death rates among both COVID-19 and non-COVID-19 hospitalized patients are likely to rise. This is the precarious edge on which the province stands.
To stem the rise in cases, the government of Ontario declared its third shutdown on Thursday. Likewise, the hospital where I have been getting my cancer care announced that it was cancelling elective surgeries. This is not due to a lack of surgeons or a lack of operating rooms. (However, I expect there is a shortage of surgical nurses due to their secondment to other COVID-related tasks.) The problem is that surgeries require hospital beds for post-operative care, including ICU beds for acutely ill patients. In effect, surgeries compete with COVID-19 for hospital beds. The upshot is that if you have a moving vehicle accident and you need a procedure right now, they will operate. Otherwise, you will wait. I’m fairly certain that they will cancel my biopsy. If so, this will delay any eventual surgery to attack my throat cancer.
So, what is it like to be a cancer patient during the COVID pandemic? Right now, it means that I cannot get the care I need. I am going to try to get more information this week about how long I can expect to wait. If it’s a long wait, or if I can’t get an answer, then I will need to explore whether I can get care in another province or, irony of ironies, in the States.

