I gave two talks at the end of last week. The first was on Accountable Care Organizations for a local chapter of the AAP. The second was on health care reform and the health care system in general. By the end of the second talk on Friday, I was pretty much feeling despondent.
As I reviewed ACOs on Thursday, I was talking about how many hoped they would bring about cost control at the physician level. But as I reviewed the progress of how the rules have been modified over time, I could feel cynicism creeping into my voice. There was the removal of sticks in October. The elimination of rules requiring EHRs. The reduction in quality oversight. The ability of patients to seek care outside the ACO. And let’s not forget the counterproductive side effect of provider concentration that the formation of ACOs encourages (Austin helpfully posted a FAQ on this balance of power earlier today).
So I’m skeptical that ACOs will be what gets us out of the ditch in the future. Not that I see many other helpful ideas from others. Tort reform won’t do what people say it will. Medicaid block grants are just passing the buck. Medicare “sorta” premium support is just cost-shifting. None of these things will get us there.
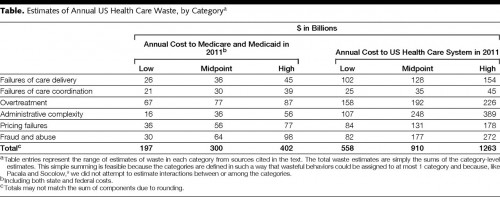
So what will, I was asked? I wish I had a magic wand to just fix things. But, more and more, I’m becoming convinced that we need to identify areas where we can save money at the local level. Wennberg’s work shows us that there are huge variations in care that don’t seem linked to quality. That stuff has to go. Berwick and Hackbarth went further and identified how much “waste” there is in the US health care system right now:
I’m drawn to the third line alone. We’re spending somewhere betweeen $156 billion and $226 billion just on overtreatment. If we could just figure out a way to stop doing that, we’d be well on our way to bending the curve. Not that we can’t fix the other things as well. But stopping overtreatment seems like it would be the easiest to do, and it would have the added benefit of not requiring that much new added infrastructure.
We may need to focus on where these things are occurring locally, though, instead of thinking there’s some large lever to pull at a national level. We also need to identify ways to change physician behavior, which isn’t easy. I’ve been talking much more about that in my own corner of the world. I hope others are, too.