I posted earlier today on some cost issues from the new paper in Health Affairs that describes a recent Commonwealth Fund survey in eleven countries. In this post, I’m going to focus more on some access-related issues from the same paper. Once again, I encourage you to go read the whole manuscript, but it may be behind a paywall for you. To summarize the methods again:
This 2010 survey examines the insurance-related experiences of adults in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United States, and the United Kingdom. The countries all have different systems of coverage, ranging from public systems to hybrid systems of public and private insurance, and with varying levels of cost sharing.
The survey consisted of computer-assisted telephone interviews of random samples of adults age eighteen or older in eleven countries, using a common questionnaire that was translated and adjusted for country-specific wording as needed. Harris Interactive and country subcontractors conducted the interviews from March though June 2010 (the field times varied by country). The final country samples, shown in Exhibit 2, ranged from 1,000 to more than 3,500.
Here we go:
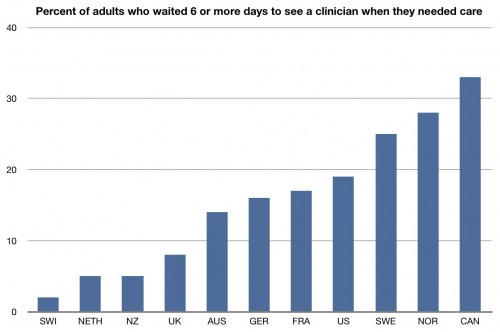
What you are looking at is the percent of adults who have to wait 6 days or more to see a doctor or nurse when they needed care. We’re not the worst; that place is held by Canada. There’s a reason that we all seem to know more about Canada’s health care system than our own. It’s because those who want to make the US look good know to whom we should compare ourselves. Yes, there are longer wait times in Canada than here for needed care. But we lose to most of the countries in this study. You have to cherry pick to make us look good.
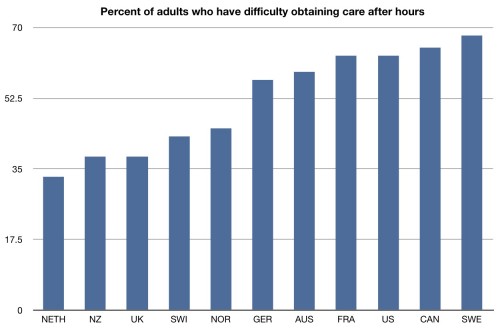
Here’s another chart that gets beyond uninsurance. This is the percent of adults who report having difficulty getting care after-hours. Almost two-thirds of people in the US have had this issue in the last year. There’s a reason for this: nights, weekends, and holidays make up a significant portion of the week. And, yet, practices in the US are not set up to deal with this. Remember that when you start to complain about overuse of emergency departments in the US. For many, many people, they are the only option when they need to get care.
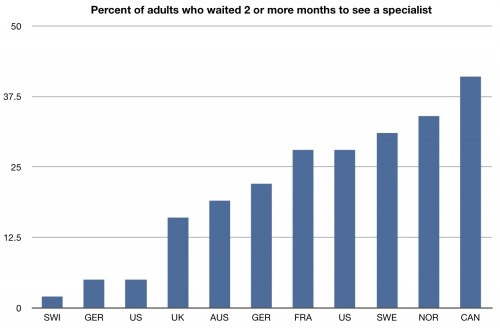
The US does well in some areas, however. Here’s one:
Few people in the US need to wait two or more months in order to see a specialist. We are much better in the rest of the world. Of course, many will say that’s contributing to our significant costs, and there’s an argument to be made that we are not seeing any quality bumps from this access.
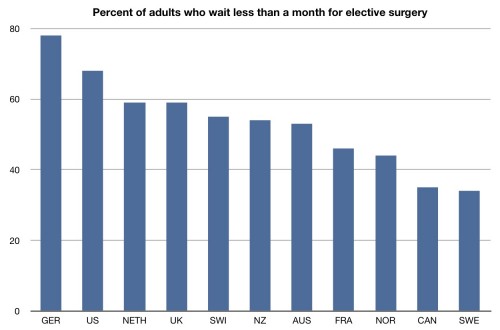
Here’s another area where we succeed:
Adults in the US report less waits for elective surgery. In fact more than two thirds of people in the US say they wait less than a month for such surgery. People in other countries have to wait longer for elective surgery.
Stop and think about all this, though. We’ve built a system where we have made it harder for people to get (relatively cheaper) care they need, and easier for them to get more expensive and elective procedures they may not. There are economic incentives that have made that happen, but it’s not helping our costs, and its not helping our quality.
People really want to keep this going?
Here’s the full manuscript: How Health Insurance Design Affects Access To Care And Costs, By Income, In Eleven Countries.