This is a TIE-U post associated with Jonathan Kolstad’s The Economics of Health Care and Policy (Penn’s HCMG 903-001, Spring 2012). For other posts in this series, see the course intro.
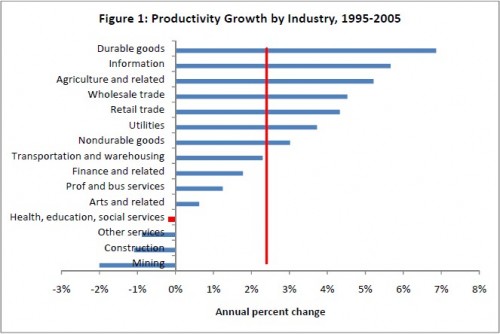
This week I’ll return to a paper by David Cutler, about which I’ve blogged before: Where Are The Health Care Entrepreneurs? The Failure of Organizational Innovation in Health Care [1]. In it, Cutler wonders why health care productivity is so low. Here’s his figure:
According to the figure, productivity growth in health, education, and social services was negative between 1995 and 2005, whereas the average across industries was 2.4%. Here’s an excerpt from another, similar figure for the period 1990-2010 from a paper by Robert Kocher and Nikhil Sahni:
(More about the Kocher and Sahni paper here.)
Cutler’s paper explains why productivity and productivity growth are low in health care and what can be done about it. He hypothesizes why we see so little innovation in health care and suggests ways to promote it. It’s a familiar set of problems (asymmetric information, inability of plans and providers to capture long-term returns on short-term investments, plan turnover, third-party payment, etc.) and solutions (bundling, provider integration, pay-for-performance, etc.). Along the way, he points to more granular evidence of low productivity: under-, over-use of care.
First under-use:
Diabetes is a chronic disease, requiring regular dietary and (often) pharmacological intervention, and testing for possible complications. There are consensus guidelines for how frequently these should occur. […]
Adherence to guideline recommendations is low. Only 43 percent of diabetics in the United States receive recommended therapy. The issue is not just lack of insurance. [… O]ther countries [with] universal coverage [have] an average success rate (46 percent) [that] is no better.
Diabetes is not unique. Only one-third of people with high blood pressure have their cholesterol under control (Cutler et al., 2008), and only one-quarter of those with high cholesterol are under control (Hyre et al., 2007). Outcomes for patients with conditions such as depression are even worse. Again, this appears similar in all countries. Unlike excessive use of care with low value, poor chronic disease care management is a feature of all developed country medical systems.
Next over-use:
Almost all elderly men have cancer of the prostate. In many cases, however, the cancer grows slowly, and the person will die of something else before the cancer becomes fatal – or even clinically meaningful. Thus, ‘watchful waiting’ is a common strategy. In some cases, the cancer will grow rapidly and should be treated. However, it is not always clear whether a patient has a rapidly growing cancer or not. […]
Some clinical evidence has examined the effectiveness of [the] different [treatment] strategies. The results suggest that the therapies are approximately equally efficacious in men aged 65 and older, the most common group diagnosed with localized prostate cancer. In particular, there is no evidence that the newer and very expensive radiation therapies have better outcomes. There is some evidence of adverse side effects with surgery – impotence and incontinence are common outcomes – making watchful waiting even more appropriate for many men.
Still, rates of invasive treatment remain high. Only 42 percent of elderly men with prostate cancer receive watchful waiting. One-third receive a radical prostatectomy, 15 percent receive brachytherapy, 1 percent receive external beam radiation therapy, and 5 percent receive intensity modulated radiation therapy. A final 4 percent of patients receive a combination of intensive treatment – which has not even been explored in the literature. […]
Patient preferences are not a major part of the variation in treatment. Sommers et al. (2008) show that patients differ in their preferences for side effects and risks of metastatis, but these preferences do not predict the therapy a patient receives. Rather, patients get referred to a particular type of specialist, and this specialist then recommends the therapy that they judge best. Thus, patients who see only a urologist most frequently undergo a radical prostatectomy, while patients seen by a radiation oncologist undergo some form of radiation.
Though we can identify reasons for low health care productivity (as above) , there is still an underlying puzzle. Why has neither market nor government found a way to wring more of the quite obvious inefficiencies from the system? Why does productivity in the health sector remain so low?
One caveat to all of the above, neither of the productivity figures illustrated account for gains attributed to changes in quality of health care. It is not the case that drugs and procedures are the same in 2000 or 2005 as they were in 1990 or 1995. Those who are consuming appropriate, necessary care are probably getting a better dose of health care than they would have a decade ago, with better health outcomes to show for it. So the productivity losses are exaggerated. By how much? I don’t know.
References
1. Cutler, D.M. “Where are the Health Care Entrepreneurs? The Failure of Organizational Innovation in Health Care” NBER WP# 16030.