Melissa Garrido, PhD is the Associate Director of the Partnered Evidence-based Policy Resource Center (PEPReC) at the Boston VA Healthcare System, U.S. Department of Veterans Affairs, and a Research Associate Professor with the Department of Health Law, Policy, and Management at Boston University School of Public Health. She tweets at @GarridoMelissa.
In the New England Journal of Medicine, Yinon Bar-On and colleagues describe the ability of a third dose of the BNT162b2 messenger RNA vaccine (Pfizer-BioNTech) to protect against severe illness and cases of Covid-19 in adults 60 or older, relative to receipt of a two-dose regimen. Although Bar-On et al.’s study leverages a unique population-level dataset, the study was observational — individuals were not randomized to receipt of the booster. As a result, unobserved variables associated with likelihood of both receiving a booster and infection, such as occupation or concern about COVID, may at least partially explain the findings.
To strengthen our ability to act upon observational data, we can use e-values. E-values characterize the degree of unobserved confounding that would need to exist before we change our inferences from an analysis. The table below includes e-values for the primary, matched, and weighted effect estimates and for the lower bounds of the confidence intervals from Bar-On et al.’s study.
Table. E-values for Bar-On et al.’s study of BNT162b2 third dose effectiveness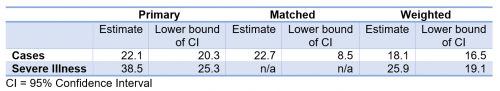
In the matched analysis, which most carefully controls for time of booster receipt, the e-value for the cases’ confidence interval lower bound is 8.5. This means that for the cases’ confidence interval to include a value of 1 (indicating no evidence of booster impact), this sample would need to include unobserved variables that are associated with both 8.5 times the likelihood of booster receipt and 8.5 times reduction in becoming infected, after controlling for the variables Bar-On et al. used.
Elsewhere, surveys of vaccine attitudes suggest a relationship between greater perceptions of Covid-19 risk and greater willingness to be vaccinated. Perceived Covid-19 risk may also lead individuals to reduce participation in activities that include a high chance of transmission. The degree to which these relationships exist in decisions about boosters and are possible confounding factors in observational studies of booster effectiveness should be clarified and acknowledged as longer-term outcomes are monitored.

