I’ve said this before, but it bears repeating. Evidence based guidelines are necessary, but not sufficient. A recent research letter in JAMA is a good example of why. It’s focusing on prostate specific antigen (PSA) screening in men older than 75 years.
For the record, no organization and no guidelines (and there are many of them) recommend screening men older than 75 with a PSA. The reason is simple. Even if they had early prostate cancer, there’s almost no way that it would be their cause of death. Since that’s the case, why put people though expensive and difficult treatments that are likely not going to change any outcomes? So for this study, the authors gathered data for primary care physicians in Texas using Medicare Part A and Part B who saw at least 20 men at least 75 years of age who didn’t have a previous diagnosis of prostate cancer. They determined each doctor’s screening rate for these men, controlling for patient characteristics. Here’s a chart of their findings:
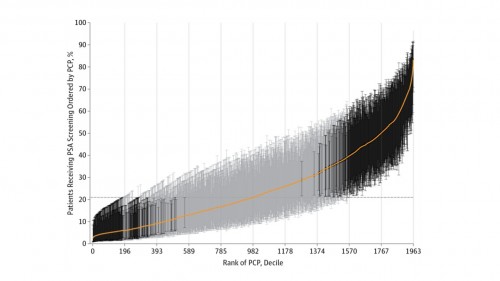 The orange line is the cumulative distribution. The horizontal dotted line is the mean screening rate , which is just over 20%. The vertical depth indicates the error bars for a 95% confidence interval. Grey lines are not significantly different from the mean. Dark lines are. Of the 1963 physicians studied, 16% were significantly lower than the mean and 24% were significantly higher than the mean.
The orange line is the cumulative distribution. The horizontal dotted line is the mean screening rate , which is just over 20%. The vertical depth indicates the error bars for a 95% confidence interval. Grey lines are not significantly different from the mean. Dark lines are. Of the 1963 physicians studied, 16% were significantly lower than the mean and 24% were significantly higher than the mean.
What’s more, it turned out that a huge predictor of whether a man over 75 years got a PSA test was which doctor he saw. In other words, it wasn’t the patients, it was the doctors.
It’s not a perfect study; no study is ever flawless. But guidelines are clear that this is not a recommended practice. Look at the variation! Some docs barely screen at all. Some docs barely don’t. And docs are the major cause of this variation, which likely leads to increased spending and potentially worse health outcomes.
We need more than just evidence.

