From JAMA Internal Medicine, “Cancer Screening Rates in Individuals With Different Life Expectancies“:
Importance: Routine cancer screening has unproven net benefit for patients with limited life expectancy.
Objective: To examine the patterns of prostate, breast, cervical, and colorectal cancer screening in the United States in individuals with different life expectancies.
Design, Setting, and Participants: Data from the population-based National Health Interview Survey (NHIS) from 2000 through 2010 were used and included 27 404 participants aged 65 years or older. Using a validated mortality index specific for NHIS, participants were grouped into those with low (<25%), intermediate (25%-49%), high (50%-74%), and very high (≥75%) risks of 9-year mortality.
Main Outcomes and Measures: Rates of prostate, breast, cervical, and colorectal cancer screening.
So let’s start with this idea: if you have a limited life expectancy, or a short time to live, then screening for some diseases really doesn’t make much sense. If cancers have a very high 10-year survival rate, then it doesn’t really pay to do much screening if you have less than 10 years to live.
This study looked at people in the National Health Interview Survey, and grouped them into risks of dying in the next 9 years. They did this using a validated mortality index designed specifically for this survey.
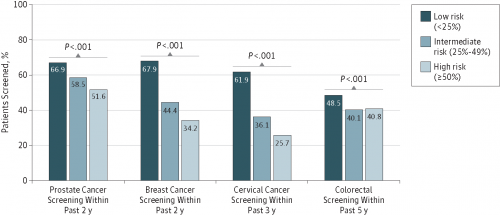
Patients with a very high 9-year mortality risk were screened for cancer quite often. Women who had had a hysterectomy were screened with PAP smears between 34% and 56% of the time within the last 3 years. Men were screened for prostate cancer at a rate of 55%. Even people who had a very high 5-year mortality risk were screened at high rates, as seen in this figure:
Bottom line is that we’re screening a huge number of people who are incredibly unlikely to receive a benefit. Why? It costs a ton of money, and it can lead to harm.