In the latest issue of Health Affairs, “Mortality Under Age 50 Accounts For Much Of The Fact That US Life Expectancy Lags That Of Other High-Income Countries“:
Life expectancy at birth in the United States is among the lowest of all high-income countries. Most recent studies have concentrated on older ages, finding that Americans have a lower life expectancy at age fifty and experience higher levels of disease and disability than do their counterparts in other industrialized nations. Using cross-national mortality data to identify the key age groups and causes of death responsible for these shortfalls, I found that mortality differences below age fifty account for two-thirds of the gap in life expectancy at birth between American males and their counterparts in sixteen comparison countries. Among females, the figure is two-fifths. The major causes of death responsible for the below-fifty trends are unintentional injuries, including drug overdose—a fact that constitutes the most striking finding from this study; noncommunicable diseases; perinatal conditions, such as pregnancy complications and birth trauma; and homicide. In all, this study highlights the importance of focusing on younger ages and on policies both to prevent the major causes of death below age fifty and to reduce social inequalities.
Then, if you’re not feeling bad enough, “Even As Mortality Fell In Most US Counties, Female Mortality Nonetheless Rose In 42.8 Percent Of Counties From 1992 To 2006“:
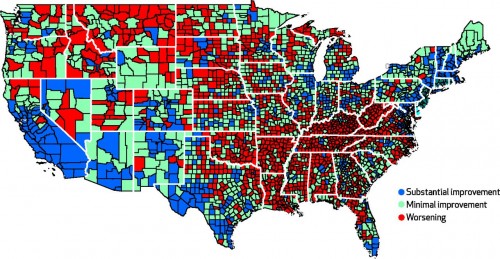
Researchers increasingly track variations in health outcomes across counties in the United States, but current ranking methods do not reflect changes in health outcomes over time. We examined trends in male and female mortality rates from 1992–96 to 2002–06 in 3,140 US counties. We found that female mortality rates increased in 42.8 percent of counties, while male mortality rates increased in only 3.4 percent. Several factors, including higher education levels, not being in the South or West, and low smoking rates, were associated with lower mortality rates. Medical care variables, such as proportions of primary care providers, were not associated with lower rates. These findings suggest that improving health outcomes across the United States will require increased public and private investment in the social and environmental determinants of health—beyond an exclusive focus on access to care or individual health behavior.
Mortality went up for women in more than 40% of counties. Seriously. Here’s the map:
Think all of those red areas are going to invest in improving “social or environmental determinants of health” anytime soon?

