“The learning health care system” is a busy space. I thank my Twitter followers for many leads. I will follow them and blog what I find useful. This is the first post. There have been prior TIE posts on this subject.
General:
- The IOM has issued many reports about the learning health care system.
- Here’s the page about a Kaiser Family Foundation convened summit on this subject.
From the IOM’s most recent report in this area, published in 2013:
- It “presents a vision of what is possible if the nation applies the resources and tools at hand by marshaling science, information technology, incentives, and care culture to transform the effectiveness and efficiency of care—to produce high-quality health care that continuously learns to be better.” (p. ix)
- “Narrow-minded rejection of scientific evidence is rarely encountered today in medicine.” (p. xi)
- “Many have pointed out a disturbing paradox: the coexistence of overtreatment and undertreatment. The committee that authored this report found a similar situation: learning and adoption that are maddeningly slow […] coexisting with overly rapid adoption of some new techniques, devices, and drugs, with harmful results.”
- The committee identified two underlying reasons for slow productivity growth in health care: (1) practitioners cannot keep up with the pace of new information, and (2) costs are rising too quickly alongside too much waste. (See p. xii.) Note that this second reason is, more or less, the definition of low productivity growth.
- New tools have emerged to attack this problem: more computational power, greater connectivity, better organizational capabilities and management science, increasing empowerment of patients. (See p. xii.) Note that the first two of these also fuel the growth in information creation and availability, which is one of the underlying problems identified. (See prior bullet.)
- Among the many best practices from other industries that could (and should) be applied to health care is “results would be routinely captured and used for continuous improvement.” (p. 6) Note that this involves a research function, to identify how to use the results to assess performance and point the way for improvement.
- Related, structuring payment incentives “to reward outcomes and value” (p. 6) implies another research role: How do we measure outcomes and value? (And what is value?)
- Here’s the committee’s schematic of today’s health care system, from page 15:

- The section on capturing opportunities from other sectors (beginning on page 16) is replete with references to “real-time knowledge,” “evidence-based,” and, of course, “continuously learning.” These are research functions. To be sure, findings need to be translated, disseminated, and implemented, but research is in the mix. It’s not all about operations management, for instance.
- Here’s how the committee conveys a learning health care system (page 19):
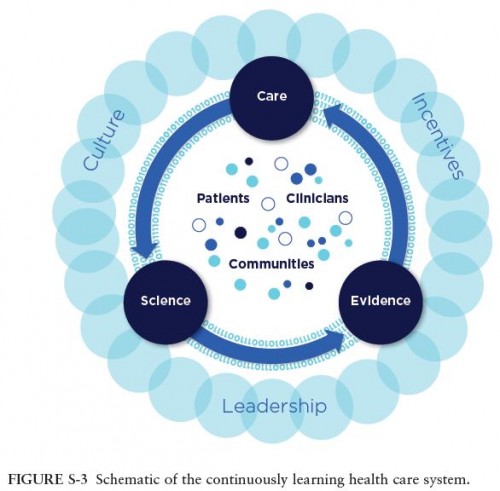
- The key distinction between figures S-3 and S-2 above is that in the latter, science and evidence (research!) are in the loop with care. Their encirclement of patients, clinicians, and communities is interesting to ponder. But leadership (which should include clinicians), culture (which clearly includes patients), and incentives (economists, basically :)), enclose the entire system. Research both informs and relies on the provision of care. The 0s and 1s just behind the curved arrows convey the flow of information. Research needs operational partners to measure and share data. Operational partners need research to assess what those data mean and what might be adjusted to move the system toward productivity goals, however defined.
- “Despite the accelerating pace of scientific discovery, the current clinical research enterprise does not sufficiently address pressing clinical questions. The result is decisions by both patients and clinicians that are inadequately informed by evidence. Meeting this challenge will require new approaches for generating clinical evidence that reduce the expense and effort of conducting research and improve the clinical applicability of research findings while retaining the rigorous reliability of the process.” (p. 20)
- “Growing computational capabilities to generate, communicate, and apply new knowledge create the potential to build a clinical data infrastructure to support continuous learning and improvement in health care.” (p. 21) In short, big data.
- “Coordination and integration of patient services currently are poor. Improvement in this area will require strong and sustained avenues of communication and cooperation between and among clinical and community stewards of services.” (p. 24) Given the pervasive multi-system use among U.S. patients, health information exchanges and natural language processing can play important roles in this area.
- “Realizing the potential of a continuously learning health care system will require a sustained commitment to improvement, optimized operations, concomitant culture change, aligned incentives, and strong leadership within and across organizations.” (p. 28) Leadership and management matter.
- Among the committee’s recommend strategies are, “Research organizations […] and care delivery organizations should facilitate the development, accessibility, and use of evidence-based and harmonized clinical practice guidelines. […] Research funding agencies and organizations should promote research into the barriers and systematic challenges to the dissemination and use of evidence at the point of care, and support research
to develop strategies and methods that can improve the usefulness and accessibility of patient outcome data and scientific evidence for clinicians and patients.” (p. 31) - Other recommended strategies include, “Health care delivery organizations […] should develop
coordination and transition processes, data sharing capabilities, and communication tools to ensure safe, seamless patient care. Health economists, health service researchers […] should develop and test metrics with which to monitor and evaluate the effectiveness of care transitions in improving patient health outcomes.” (p. 33) Also, “Health economists, health service researchers […] should partner with public and private payers to develop and evaluate metrics, payment models, contracting policies, and benefit designs that reward high-value care that improves health outcomes.” (p. 34)
It’s clear from all this that research and operations need to be in the loop with one-another to meet the committee’s recommendations. It would be inaccurate to call the resulting structure merely a management activity or solely a research one. It has aspects of both (Figure S3). They should not be siloed (Figure S2).
That’s all from the summary. Additional details, which I did not read, are in the remainder of the 400+ page report.


