My recent post on Japan drew quite a few skeptical comments, in addition to some supporting Japanese health care. Japan does indeed provide universal coverage through private plans at half the cost. Plus one of the very best life expectancies in the OECD.
How? From the latest installment in The Lancet’s six-part series on the Japanese health system:
Japan’s premier health accomplishment in the past 50 years is the achievement of good population health at low cost with increased equity between different population groups. Shibuya K, et al. Future of Japan’s system of good health at low cost with equity: beyond universal coverage. The Lancet 2011;378:1265-1273.
Just look at the title of that article. US health policy can only dream about being so lucky. In the US we increasingly specify how care must be delivered:
A concern about universal coverage is how to control health expenditures in a sustainable manner. Japan’s basic policy has been a combination of tight supply-side control for the conditions of payment with the fee schedule, with a laissez-faire approach to how services are delivered.
Some of the comments claim “Japanese exceptionalism” often with cultural or genetic explanations. Another possibility is the Japanese produce health care more efficiently, like cars.
Are they too frugal? Consider how they reimburse for drugs (WSJ) (h/t to Brad F):
Part of the attraction: with Japan’s rapidly aging population—23% of which is 65 years or older, more than any developed country, according to data from the country’s health ministry—demand for health care is expected to grow substantially in coming years. Tokyo also has eased some of the barriers that used to frustrate foreign drug makers trying to introduce new medicines.
Perhaps Tokyo’s most important move has been changing the way the national health plan reimburses for brand-name drugs. The government insurer has mandated that a branded drug’s price be cut every two years, usually by an average 4% to 7%, which industry officials say discourages the introduction of many new drugs. Last year, Japan started a pilot program to exempt certain innovative medicines from that requirement.
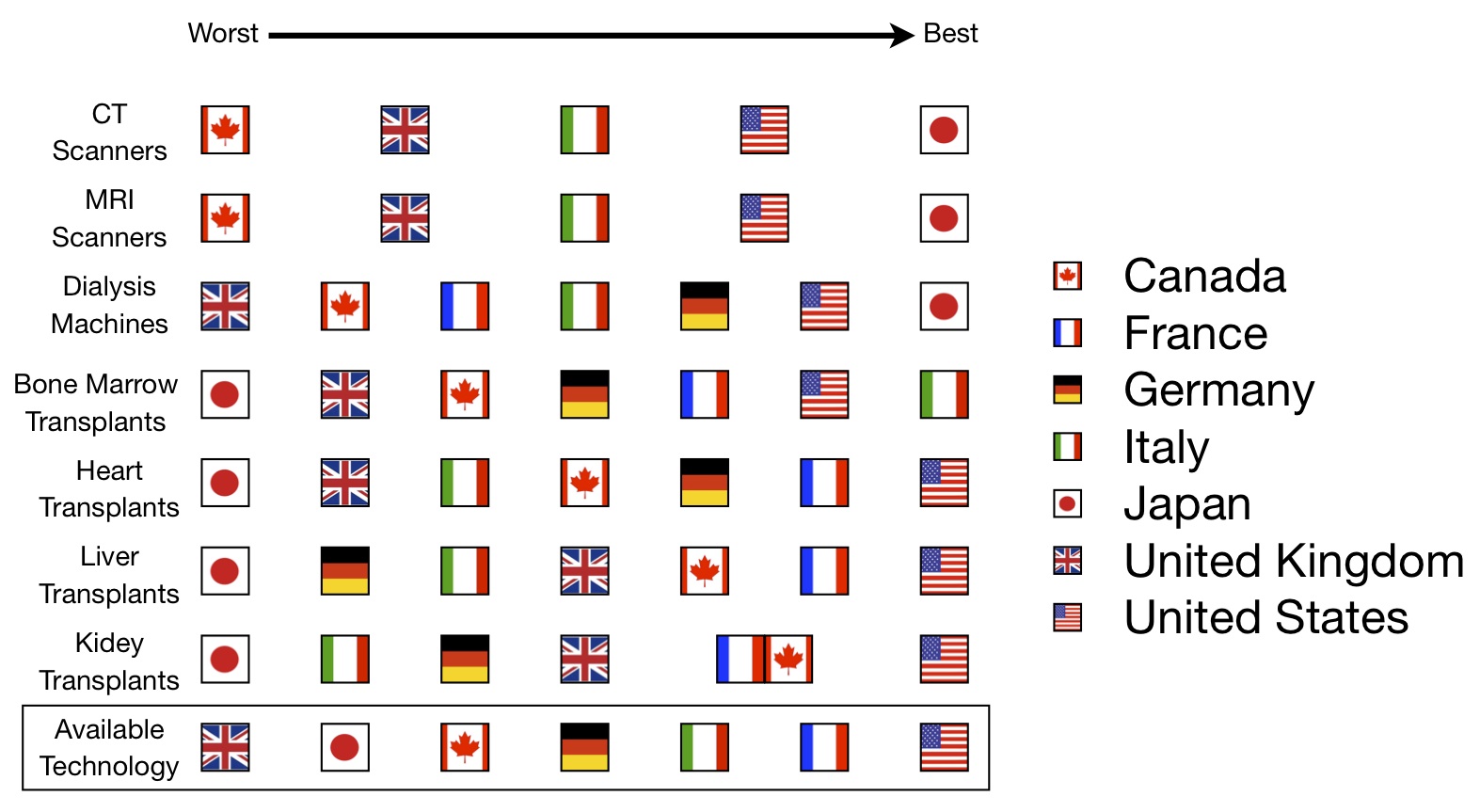
Finally, remember Aaron’s famous cross-national comparison posts? For technology access, Japan rated best in some categories and worst in others: