“Supply sensitive care” is health care delivered at a volume that responds to availability of provider supply and in ways that cannot be explained by other factors like the health of the patient population. Of course all care is supply sensitive to some extent, but some things are more so than others, particularly when there is a lack of evidence or guidelines to inform best practice.
This Dartmouth Atlas project topic brief (pdf) on the subject is a quick and easy read. Here’s just one illustration from it:
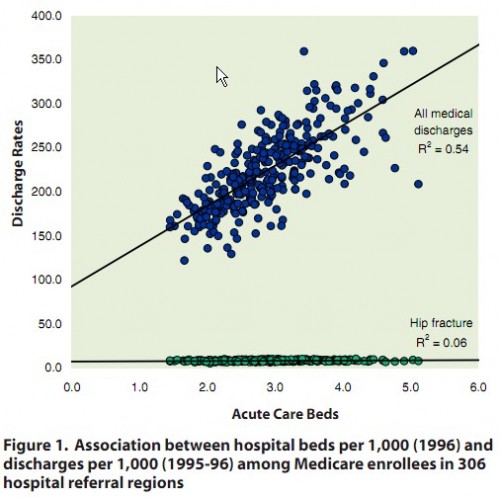
The blue dots represent how hospitalization (discharge) rates for non-surgical conditions vary with number of acute care beds across 306 regions of the US (hospital referral regions). The green dots are for hip fractures, for which hospitalization is indisputably warranted. For hip fractures,
the hospitalization rate is similar across the country, with no correlation to the supply of hospital beds. By contrast, more than half of the variation in hospitalization rates for medical (non-surgical) conditions is associated with bed capacity.
There’s a huge literature on regional variations in health spending, which I won’t review here. (See Bernstein, Reschovsky, and White and/or the CBO, both ungated PDFs.) It’s natural to ask to what extent any of it could be due to patient preferences, for instance cultural differences that drive variation in the demand for care and care intensity. That’s a difficult question to address.
Amber Barnato and colleagues take it on in Are Regional Variations in End-of-Life Care Intensity Explained by Patient Preferences? (ungated PDF). They conducted a survey of Medicare beneficiary and elicited responses to questions about preferences pertaining to end-of-life care.
Outcomes included concern about receiving too little medical treatment in the last year of life or receiving too much medical treatment, preference for dying in an acute care hospital, for life-prolonging drugs with side-effects, for palliative drugs with potential for life-shortening, and for mechanical ventilation.
They did not find a relationship between patient preferences and end-of-life spending.
We did not find a pattern of greater concern about receiving too little medical treatment, less concern about receiving too much medical treatment, preference for spending one’s last days in a hospital, for life-prolonging drugs despite side-effects, and for mechanical ventilation to achieve 1 week’s and 1 month’s life extension across respondents living in regions with progressively greater EOL spending. The observed relationship between respondents’ preferences for avoiding potentially life shortening palliative drugs and greater spending regions was explained by the confounding effect of race/ethnicity. Taken together, the lack of cross-sectional association between preferences and spending in our study is unsupportive of the hypothesis that differences in preferences explain regional variations in EOL spending. […]
In summary, the results of this survey do not support the hypothesis that observed regional variations in EOL spending are attributable to differences in goals and preferences for care among residents of those regions.
If the study findings can be extrapolated to care other than at the end of life, patient preferences have very little to do with geographic variation in health spending. If it’s not a demand phenomenon, then it must be a supply one. Care and care intensity seem to be driven in large part by the level of supply, though there are other factors. If you build it, offer it, and certainly if you promote or prescribe it, they will come and Medicare, as well as private insurers, will pay, whether it is good for health or not.
Expect many more posts on these subjects in the near term (this week and next), and likely for months and years to come. In particular, next week I’ll explain the difference between supply sensitive care and supplier-induced demand.
AF