The following was originally posted on the AcademyHealth blog earlier this year.
I highly recommend the recent paper in The Milbank Quarterly by Harvard health economists Joseph Newhouse and Tomas McGuire on the cost, beneficiary selection (as in favorable vs. adverse), market power, and quality of Medicare Advantage (MA). Just as it sounds, it summarizes just about everything a wonk might want to know about the program. In this post, I will make just three points articulated in the paper.
Historically, the case against MA was easy: it cost too much and quality was uncertain and, possibly, suspected to be no better or worse than traditional Medicare (TM). (See the work of Miller and Luft.) More recent data compels at least a partial reassessment of the program. Newhouse and McGuire make, perhaps, one of the stronger, evidence-based cases in its favor I’ve read in a long time.
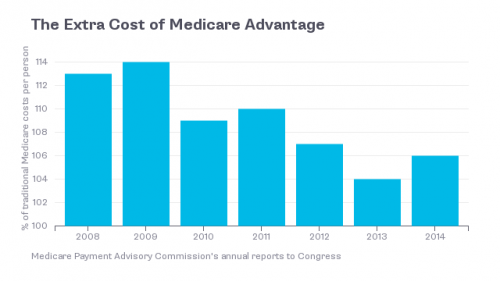
First, yes, MA plans are still overpaid relative to the cost of providing the Medicare benefit via TM. This is nicely illustrated in the chart below, from Bloomberg View.
But things are at least slightly less bad than they appear. As found by Kate Baicker, Mike Chernew, and Jacob Robbins and explained by Newhouse and McGuire, there is a spillover effect whereby MA causes offsetting savings for TM, as well as in the commercial market. (An earlier version of their publication exists as an NBER working paper as well, which I summarized.)
We find that when more seniors enroll in Medicare managed care [an MA plan], hospital costs decline for all seniors and for commercially insured younger populations. Greater managed care penetration is not associated with fewer hospitalizations, but is associated with lower costs and shorter stays per hospitalization. These spillovers are substantial – offsetting more than 10% of increased payments to Medicare Advantage plans. […]
So, that’s not a total offset to the extra MA cost, but it’s a little off the top.
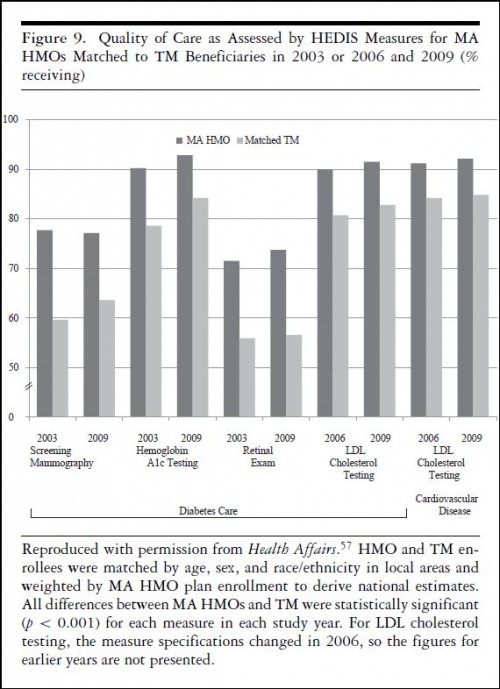
Next, Newhouse and McGuire share results from a paper by John Ayanian and colleagues that demonstrates that MA offers higher quality than TM, at least in the dimensions measured. The chart just below shows the proportion of beneficiaries in a Medicare Advantage HMO and TM receiving each of several preventive services. Women enrolled in an HMO are more likely to receive mammography screening,* those with diabetes are more likely to receive HbA1c testing, retinal exams, and those with diabetes or cardiovascular disease are more likely to receive cholesterol testing.
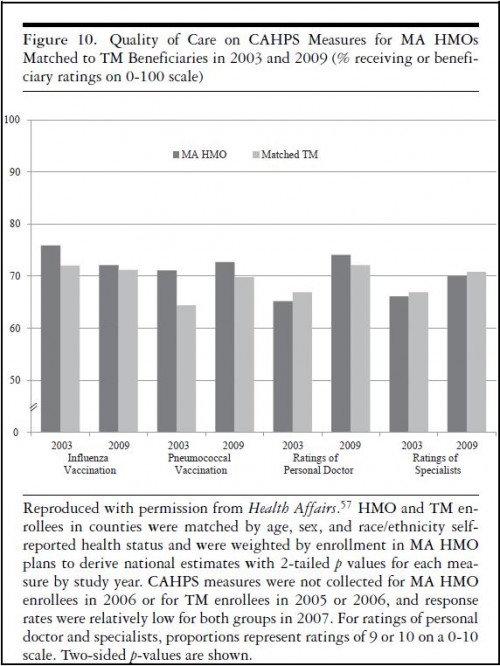
The next chart shows that HMO enrollees are more likely to receive flu and pneumonia vaccinations and about as likely to highly rate their personal doctor and specialists.
Finally, Newhouse and McGuire point to both published and unpublished work by Bruce Landon and colleagues that finds reduced resource use (which they call “social cost”) by beneficiaries in MA plans.
Rates of ambulatory surgery and emergency department use were 20% to 30% lower in the MA plans [relative to TM]. The difference was concentrated in elective procedures regarded as more “discretionary,” such as knee or hip replacements. Repair of a fracture of the femur, a less discretionary procedure, was actually greater in MA.
Minimizing social cost also involves using more durable procedures if equally effective. Landon and colleagues found that coronary problems were more frequently treated with coronary bypass surgery in MA rather than the less durable percutaneous coronary intervention, suggesting not just lower long-run costs on average but a more appropriate use of services, since the patient was potentially spared a repeat procedure.
They go on to describe other work illustrating reduced social cost in MA.
In conclusion, Newhouse and McGuire wrote,
We found several reasons to maintain the level of payment to MA plans at or above the level of TM. First, the quality and appropriateness of care appear to be at least as high in MA as in TM. Second, the social cost of care in MA appears to be lower than in TM. Third, we found evidence for positive “spillovers,” meaning that higher MA enrollment in a county reduces hospital costs in TM in that county. Medicare does not immediately capture the savings, since it pays per admission (unless an admission without a procedure replaces one with a procedure). Rather, the savings would have to be captured later by a smaller update factor. Reducing the percentage of the benchmark paid to MA plans, as was done in the ACA, generates program savings for Medicare, but from the standpoint of the Medicare program’s social efficiency, cuts in MA plan payments may be shortsighted.
This is somewhat hedged, but I’d hedge further because a full welfare analysis has not been done to justify a specific MA payment level, relative to TM. It’s possible that MA is still overpaid from a social perspective, and we don’t know by how much.
There’s a lot more in the paper. I recommend you read the whole thing.
* According to the original paper, this measure applies to all women, not just those receiving diabetes care as suggested in the chart.