Awesome, awesome article in the NYT over the weekend on whether MRIs are really useful in diagnosis. The piece describes two studies. Here’s the first:
Dr. Green and his colleagues reviewed the records of 101 patients who had shoulder pain lasting at least six weeks and that had not resulted from trauma, like a fall. Forty-three arrived bearing M.R.I.’s from a doctor who had seen them previously. The others did not have scans. In all cases, Dr. Green made a diagnosis on the basis of a physical exam, a history, and regular X-rays.
A year later, Dr. Green re-assessed the patients. There was no difference in the outcome of the treatment of the two groups of patients despite his knowledge of the findings on the scans. M.R.I.’s, he said, are not needed for the initial evaluation and treatment of many whose shoulder pain does not result from an actual injury to the shoulder.
Now this isn’t a randomized controlled trial, and I could pick apart the methodology if someone wanted to make grand pronouncements based on the results. But let’s accept that this study shows it’s possible to treat patients equally well in this situation with or without an MRI.
Here’s the second study:
Dr. DiGiovanni did a similar study with foot and ankle patients, looking back at 221 consecutive patients over a three-month period, 201 of whom did not have fractures. More than 15 percent arrived with M.R.I.’s obtained by doctors they had seen before coming to Dr. DiGiovanni. Nearly 90 percent of those scans were unnecessary and half had interpretations that either made no difference to the patient’s diagnosis or were at odds with the diagnosis.
Part of the problem is that so many of these MRIs are just unnecessary. Some doctors get them because that’s how they were trained. Some get them because they think patients want them and see them as part of “quality” care. Some doctors get them because they think it will protect them from getting sued.
When tests like the MRI are first developed, they are used on specific people who are very likely to have specific issues, to order to prove they work. Later, however, they get used on a broader and broader population. The problem, though, is that we often have no idea how these tests will work on a healthy population. We don’t know how many normal people might have abnormal MRIs. So you get into situations like these:
Dr. James Andrews, a widely known sports medicine orthopedist in Gulf Breeze, Fla., wanted to test his suspicion that M.R.I.’s, the scans given to almost every injured athlete or casual exerciser, might be a bit misleading. So he scanned the shoulders of 31 perfectly healthy professional baseball pitchers.
The pitchers were not injured and had no pain. But the M.R.I.’s found abnormal shoulder cartilage in 90 percent of them and abnormal rotator cuff tendons in 87 percent.
Remember that these are top athletes, who have some of the best functioning shoulders in the world. Almost 9 in 10 of them have abnormal MRIs. As Dr. Andrews remarks, “If you want an excuse to operate on a pitcher’s throwing shoulder, just get an M.R.I.” Do you think these pitchers would benefit from surgery? Do you think it would have been good for them to get MRIs in their doctors’ offices?
This is a real problem in American medicine. We really seem to value this stuff. We even prioritize it:
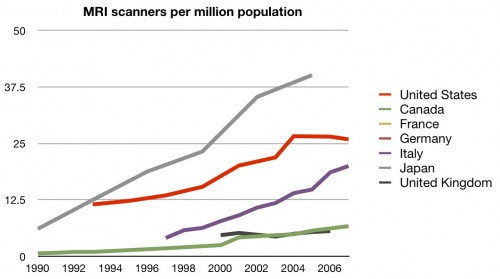
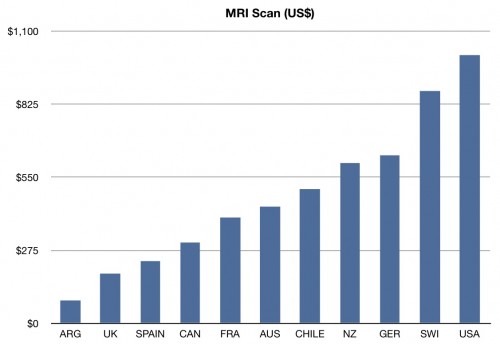
We are second only to Japan in the number of MRIs per population. We also charge much more for them than pretty much any other country, according to the International Federation of Health Plans’ Annual Comparative Price Report. :
 So here in the US we’ve got a test that’s over-utilized, over-charged, and that likely leads to large numbers of false-positives, requiring even more expense and likely increased harm. But the MRI is just one example of a huge problem that encompasses the overuse of all kinds of technology and screening here. It’s one we’re still denying, and one that we will need to confront if we have any hope of improving our health care system.
So here in the US we’ve got a test that’s over-utilized, over-charged, and that likely leads to large numbers of false-positives, requiring even more expense and likely increased harm. But the MRI is just one example of a huge problem that encompasses the overuse of all kinds of technology and screening here. It’s one we’re still denying, and one that we will need to confront if we have any hope of improving our health care system.