Not too long ago, antibiotic prophylaxis would be given before various procedures, like going to the dentist to people at risk for infective endocarditis. This applied to people at both high and low risk. Full disclosure, I’m one of the people at low risk, and I used to have to take antibiotics before such things, and I had to take azithromycin (which hurts my belly) cause I’m allergic to penicillin, and it sucked. Sorry – had to vent. So, anyway, I was pleased when research changed the guideline for people at low risk, and I could stop taking the drug.
And then Brad Flansbaum sent me this. “Incidence of infective endocarditis in England, 2000—13: a secular trend, interrupted time-series analysis“:
Background: Antibiotic prophylaxis given before invasive dental procedures in patients at risk of developing infective endocarditis has historically been the focus of infective endocarditis prevention. Recent changes in antibiotic prophylaxis guidelines in the USA and Europe have substantially reduced the number of patients for whom antibiotic prophylaxis is recommended. In the UK, guidelines from the National Institute for Health and Clinical Excellence (NICE) recommended complete cessation of antibiotic prophylaxis for prevention of infective endocarditis in March, 2008. We aimed to investigate changes in the prescribing of antibiotic prophylaxis and the incidence of infective endocarditis since the introduction of these guidelines.
Methods: We did a retrospective secular trend study, analysed as an interrupted time series, to investigate the effect of antibiotic prophylaxis versus no prophylaxis on the incidence of infective endocarditis in England. We analysed data for the prescription of antibiotic prophylaxis from Jan 1, 2004, to March 31, 2013, and hospital discharge episode statistics for patients with a primary diagnosis of infective endocarditis from Jan 1, 2000, to March 31, 2013. We compared the incidence of infective endocarditis before and after the introduction of the NICE guidelines using segmented regression analysis of the interrupted time series.
They basically looked at all of England to see what’s been happening with infective endocarditis since 2004. NCE guidelines were put in place in 2008 to stop using antibiotic prophylaxis. Now, they stopped it for everyone, even those at high risk.
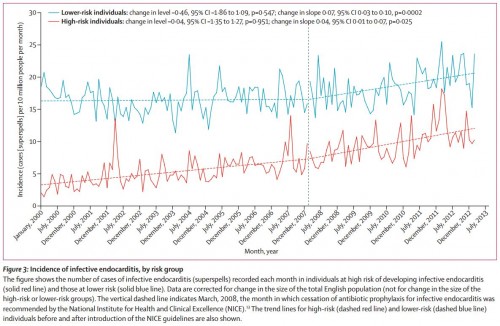
The guidelines worked as intended. Prescriptions fell from an average of almost 11,000 per month before the change to just over 2200 a month after. But, starting with the change, the number of cases of infective endocarditis started going up. Not by huge numbers, but by March, 2013, they had 35 more cases of infective endocarditis than would have been predicted by secular trends alone. What has me really concerned is that cases increased both for those at high and low risk:
This isn’t causality, and it’s not time to panic. But it’s worth looking at in other places. Did we make the right call in ending this practice? The NICE is reviewing its guidelines.
UPDATE #1: Ok, why is the incidence of endocarditis so much higher in the low risk population than in the high risk population? Both before and after guideline changes? That’s crazy. I emailed the author to ask about it, and I will post the answer when I get it.
UPDATE #2: Dr. Martin Thornhill, one of the authors of the paper, responds to my question. Here is his answer (with permission):
Yes it is concerning as it raises questions not just with regard to the NICE guidelines but also with regard to other guidelines such as the AHA and ESC. A possible reason why the increase was greater in low-risk individuals than High-risk individuals may be because we have underestimated the effect in high-risk individuals. It is important to note that there are still over a 1000 antibiotic prophylaxis prescriptions per month being issued and we know from other research that we have done that these are principally targeted at high-risk individuals I.e. Despite the fall in AP in the UK a proportion of high-risk individuals are still receiving AP. It is very important to remember, however, that we cannot assume a cause and effect relationship between these increases in IE incidence and the changes in antibiotic prophylaxis prescribing.
If I’m understanding this correctly, the reason that the rate of endocarditis is lower in high risk individuals may be because they are still getting prophylaxis. The question at the end of my original post still holds, except now I’d like to ask it a little louder!