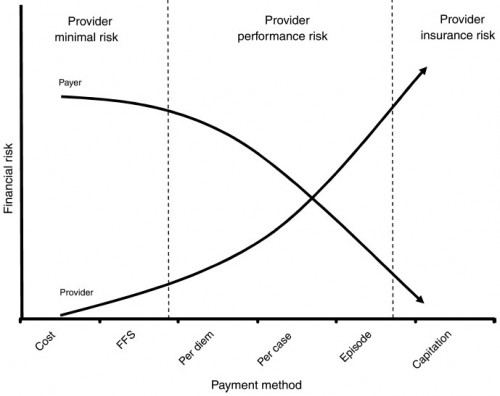
I like this figure from “Achieving Cost Control, Care Coordination, and Quality Improvement through Incremental Payment System Reform” (Averill, et al., JACM, 2010).
The third dimension would be risk borne by the insured (degree of cost-sharing or “consumer directed-ness”). The paper describes various Medicare payment reform methods. Here’s the abstract:
The healthcare reform goal of increasing eligibility and coverage cannot be realized without simultaneously achieving control over healthcare costs. The reform of existing payment systems can provide the financial incentive for providers to deliver care in a more coordinated and efficient manner with minimal changes to existing payer and provider infrastructure. Pay for performance, best practice pricing, price discounting, alignment of incentives, the medical home, payment by episodes, and provider performance reports are a set of payment reforms that can result in lower costs, better coordination of care, improved quality of care, and increased consumer involvement. These reforms can produce immediate Medicare annual savings of $10 billion and create the framework for future savings by establishing financial incentives for long-term provider behavior changes that can lead to lower costs.