In NEJM, Robert Huckman and Mark Kelley wrote:
Between 2006 and 2012, the prevalence of high-deductible health plans grew by 24%, exposing one third of privately insured employees to deductibles of at least $1,000. Copayments have shown similar growth, with nearly half of covered employees paying $25 or more for an office visit.
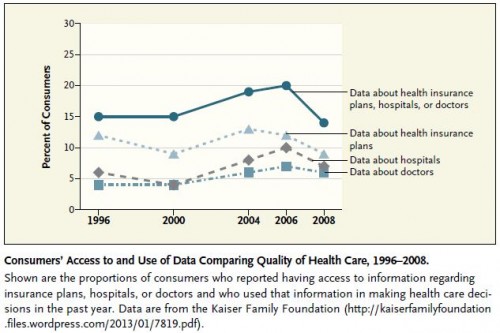
On the hook for greater cost, was there a surge of use of quality data by consumers since 2006? Nope:
OK, this chart doesn’t show us what might have happened after 2008. So, maybe there has been an upward surge of quality data use more recently. I doubt it, but I certainly could be wrong about that.