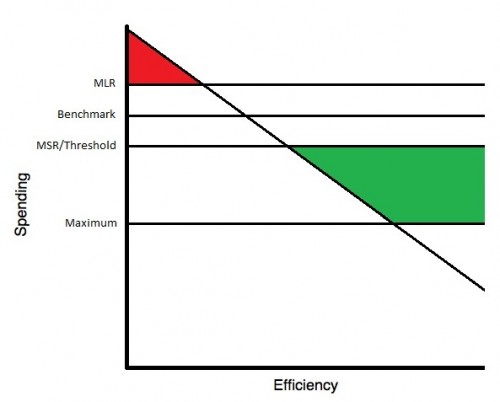
I’m getting a lot of emails, so I’m going to break it down even further. Here’s how the ACO payments and penalties work. Let’s start with the diagrams. First up is the one-sided ACO:
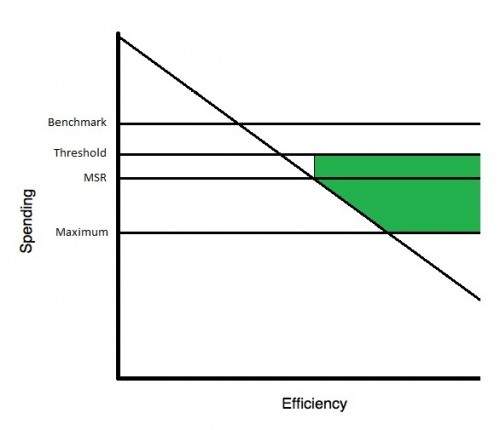
And now the two-sided ACO:
Let’s get oriented. Spending is on the y-axis. The diagonal line shows increasing efficiency of ACOs as you move from left to right. More efficient ACOs (further to the right) will spend less relative to their benchmark. What’s a benchmark? OK, let’s get into it.
The benchmark is what HHS says an ACO should spend. So if an ACO spends more than the benchmark, they spent too much. They’re inefficient. If they spent less than the benchmark, then they saved money. They were efficient. (This efficiency/inefficiency terminology is mine, not HHS’s. I just find it useful to think about it that way. But, an ACO could “overspend” at random too. They could have a bad year, have a lot of sicker than normal patients. Same goes for efficiency. It could be luck once in a while.)
Every ACO is also assigned a sharing rate based on their quality performance and whether they have members who use a Federally Qualified Health Center or Rural Health Center. The sharing rate is the proportion of the savings that the ACO generates that they could get back in revenue. The government keeps the rest. For a one-sided ACO, the maximum sharing rate is 52.5%. For two-sided ACOs, the maximum sharing rate is 65%. That’s on the savings side. For two-sided ACOs, which face penalties, the sharing rate on penalties is (1-sharing rate on savings).
The MLR is the Minimum Loss Rate. It is a percentage of the benchmark. If a two-sided ACO spends more than (benchmark + MLR) (or, in words, more than MLR over the benchmark), then they must pay the government back (1-sharing rate on savings) *spending above the MLR line. That’s the red. It maxes out depending on year, but even in year three, no ACO would owe more than 10% of the benchmark. One-sided ACOs never owe a penalty (which is why there’s no red on the one-sided ACO diagram). That’s the difference between a one- and two-sided ACO.
The MSR is the Minimum Savings Rate. For two-sided ACOs, this is always 2% of the benchmark. For one-sided ACO’s, it’s at least 2% and dependent on the size of the ACO. For spending between the (benchmark+MLR) and (benchmark-MSR), no penalties or bonuses are paid. Once spending drops below (benchmark-MSR), however, the ACO starts to earn a bonus (green). It’s calculated by the spending below the (benchmark-threshold) times the sharing rate. For two-sided ACOs, the threshold equals the MSR (2%), so they earn more earlier. Bonuses cap out at a maximum equal to 7.5% of benchmark for one-sided ACOs and 10% of benchmark for two-sided ACOs.
Hope this helps!