In the past two decades, Medicare’s administrators have conducted demonstrations to test two broad approaches to enhancing the quality of health care and improving the efficiency of health care delivery in Medicare’s fee-for-service program.Disease management and care coordination demonstrations have sought to improve the quality of care of beneficiaries with chronic illnesses and those whose health care is expected to be particularly costly. Value-based payment demonstrations have given health care providers financial incentives to improve the quality and efficiency of care rather than payments based strictly on the volume and intensity of services delivered.
In an issue brief released today, CBO reviewed the outcomes of 10 major demonstrations—6 in the first category and 4 in the second—that have been evaluated by independent researchers. CBO finds that most programs tested in those demonstrations have not reduced federal spending on Medicare.
One way the programs were to save money was to prevent admissions to the hospital by doing a better job in the outpatient setting. Here’s how they did:
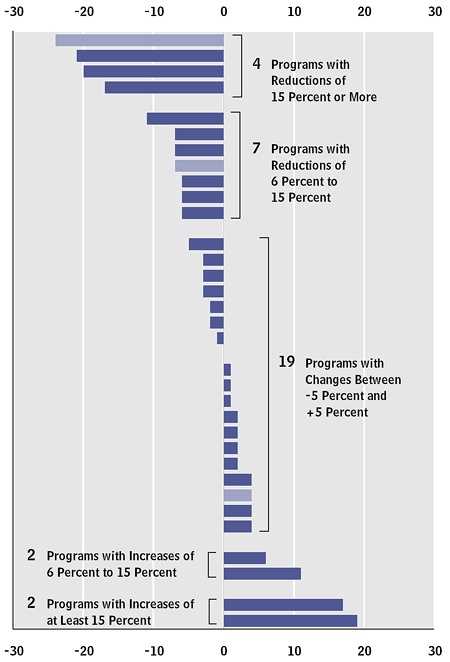
On average, there was no real effect. Moreover, in pretty much every program, spending was either unchanged or increased compared to what would have occurred without them. One of the few positive notes was that programs with care managers who were assigned to have more direct interaction with physicians and patients were more likely to show spending decreases than other programs. Even then, though, those spending reductions weren’t enough to compensate for their fees.
The conclusion:
Demonstrations aimed at reducing spending and increasing quality of care face significant challenges in overcoming the incentives inherent in Medicare’s fee-for-service payment system, which rewards providers for delivering more care but does not pay them for coordinating with other providers, and the nation’s decentralized health care delivery system, which does not facilitate communication or coordination among providers. The results of those Medicare demonstrations suggest that substantial changes to payment and delivery systems will probably be necessary for programs involving disease management and care coordination or value-based payment to significantly reduce spending and either maintain or improve the quality of care provided to patients.
We’ve got a lot of work to do. It would be nice to see some policymakers specifically discussing these issues, or how we might address them. Just repeating that “we will pay for quality, not quantity” isn’t enough. I’m looking at both sides here.

