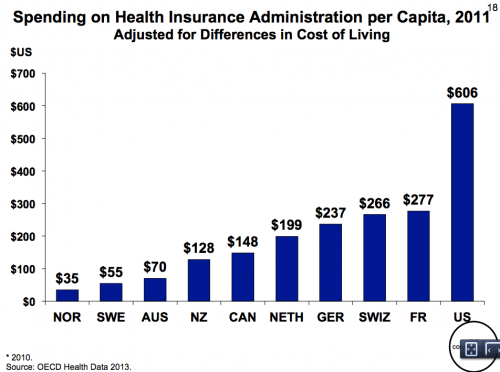
Here’s a graph I posted yesterday that shows that the cost of health care administration is much higher in the US than in comparable countries.
So where does this excess administrative cost come from? I have a story from a meeting I was in this morning that will give you a sense of the problem and why it matters.
I’m at my US job this week and the day’s project is to measure the quality of care delivered by a large pediatric Accountable Care Organization (ACO). We want to know, for example, whether the kids have all their vaccinations. This seems like a simple question. When a kid gets his shot, his doctor submits a claim to the kid’s insurer for the service. So just pull together all the claims, count the kids who have claims for a vaccination, and divide by the number of kids in the system. Then you know what proportion of the kids have been vaccinated. Right?
Uh, no. To understand why not you need to, of course, follow the money. The money starts with the state Medicaid office. From there, it goes to five managed care organizations (MCOs). Because the MCOs never learned how to actually, like, manage care, they subcontract their business to the ACO. The ACO then works directly with the physicians. You can see a source of waste right away, because money passes through too many middlemen on the way to the doctors. It’s also a pain for the doctors who have to deal with the ACO and multiple MCOs, each asking for information on their own forms.
Still with me? Recall that the ACO, which is responsible for the quality of care, wanted to use these claims to determine whether the kids have gotten their shots. The next problem is that the claims only come to the ACO from the MCOs after the MCO is finished processing them, which can take months.
Worse, you have to match claims to kids using patient IDs, and each claim has a patient ID that is specific to that MCO. Unfortunately, kids often switch from one managed care plan to another, at which point the kid gets a new ID. This means that the same kid can appear in the data under multiple identifiers. But to determine whether the kid got all of his shots, you need to look at all his claims, and this means that you have to reconcile the multiple IDs. This takes work, the matching is never completely accurate, and the process slows everything down even more.
The delay and needless processing add cost to the system and noise to the eventual quality measure. Measuring quality of care is a dry, tedious topic, but it’s incredibly important.
The problem I’m dealing with is a problem of Medicaid. But it is not a problem unique to Medicaid and some of the overlapping financial entities arose from previous attempts to privatize aspects of the system. The next round of reformers need to strive for simplicity.