In Medical Care, Yu-Chu Shen and Vivian Wu have published a nice study of the effect on patient outcomes of Medicare hospital payment reductions. They exploit changes made by the Balanced Budget Act (BBA) of 1997 and subsequent payment policy changes, which are similar to some, but not all, of the changes in Medicare hospital payments made by the Affordable Care Act.
The BBA and ACA both lower hospital spending primarily by reducing diagnosis-related group (DRG) payment increases. However, the scale of payment reduction contained in ACA is larger: the BBA reduced Medicare inpatient payment by about 5% between 1998 and 2000, whereas the ACA will reduce DRG payment by an estimated 1.1% per year indefinitely.
The BBA cuts were subsequently reversed, but the totality of the policy changes was to split hospitals into relatively lower- and higher-payment groups. What did this difference in payments do? They killed people.
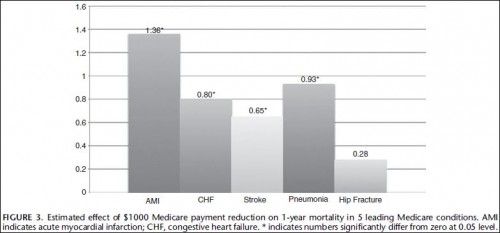
Figure 3 shows the estimated effect of a $1000 Medicare payment cut on 1-year mortality for the 5 conditions, based on the second model. If payment per Medicare patient for a hospital were to reduce by $1000, the 1-year mortality rate would be expected to increase by 1.36 percentage points for AMI (95% CI, 0.73–1.98), 0.80 percentage point for CHF (95% CI, 0.28–1.32), 0.65 percentage point for stroke (95% CI, 0.02–1.27), and 0.93 percentage point for pneumonia (95% CI, 0.42–1.44).
So, this is not good from a keeping-people-alive point of view. But we can tolerate other points of view here, and Shen and Wu offer one.
[H]ow does the cost of life loss compare to the benefit of financial savings? […] Following Figure 3, we estimated a 1.36-percentage point increase in 1-year mortality for every $1000 payment reduction per [AMI] hospital discharge, which implies that 7353 lives were lost during the study period []. When combining the 4 conditions where we found a significant effect—the total saving to Medicare is $7.26 billion, at the expense of 39,477 lives.
Figuring that a typical Medicare beneficiary is about 72 years old and has a life expectancy on the order of 10 years,* the loss in life represents roughly a half-million lost life years, at a savings of $7.26 billion, or about $15,000 per life-year. Granted, a life-year is not a quality adjusted life-year, but this is well below typical estimates for what we are willing to pay for one. So, even from a hard-nosed, economist’s point of view, the BBA cuts were costly, at least according to this study.
Will the ACA’s other attempts to enhance quality offset the damage its Medicare hospital payment cuts may do? This is an open and important question.
* Maybe a bit longer. I’m being conservative. See Table 18 in this PDF.
UPDATE: Edited to clarify that the findings are not based on BBA cuts per se, but on the difference between lower and higher hospital payments stemming from the BBA and subsequent policy changes.