To understand and manage Medicaid spending requires analysis of Medicaid enrollees with substance use disorder. A GAO report released in May implicitly makes the case.
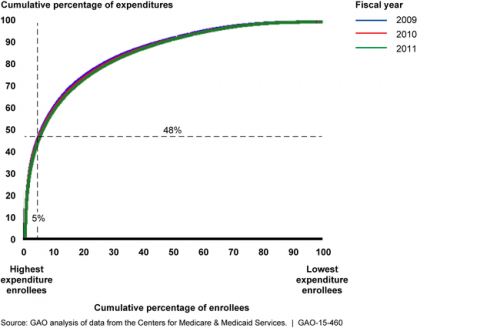
The first thing one learns from the report is just how skewed the Medicaid distribution of spending is. For instance, the top 5% most expensive Medicaid enrollees* account for nearly half of all Medicaid spending. (Really, we knew this already. All health care spending is similarly skewed, whether Medicaid or not.)
On page 11 of the report we learn that the most costly Medicaid enrollees disproportionately have a substance use disorder: Of the 5% most costly Medicaid enrollees, one in five have one, whereas across all Medicaid enrollees fewer than one in 20 do.
On page 13 we learn that substance use is intimately related to mental health conditions, but even more so for the most costly enrollees. Among the 5% most costly enrollees, 71% of those with a substance use disorder also have a mental health condition. Medicaid-wide, the figure is 51%.
I doubt the basic story changes much if one examines the top 10% most expensive enrollees (who account for about 65% of spending) or the top 20% (accounting for about 80% of spending). Substance use disorder is key.
High cost enrollees are where the money is, nearly all of it. Given this, one isn’t going to make a lot of progress understanding and managing high cost Medicaid enrollees without data on those with substance use disorders. The trouble? Those data are no longer available to researchers the way they have been for decades.
(If you’re the least bit surprised by this, welcome to TIE. Catch up on the substance use disorder data suppression issue with these posts.)
* The GAO report considers only Medicaid enrollees not also enrolled in Medicare. Every use of “Medicaid enrollees” in this post should be interpreted accordingly.