Imagine:
Until 1961, patients with acute myocardial infarction — if fortunate enough to survive until they reached a hospital — were placed in beds located throughout the hospital and far enough away from nurses’ stations that their rest would not be disturbed. Patients were commonly found dead in their beds, presumably from a fatal tachyarrhythmia. Indeed, the risk of death occurring in the hospital was approximately 30%.
That’s from “A Tale of Coronary Artery Disease and Myocardial Infarction,” by Elizabeth Nabel and Eugene Braunwald (NEJM). We have come a long way since 1961. Improvement in care for patients with cardiovascular disease is one of the great medical success stories of the 20th century, complementing great strides in public health. We owe this triumph of medicine to the interdisciplinary efforts at enhancement to the technology of care (from devices to drugs to surgical technique), evidence from clinical trials, and dissemination of best practice and lifestyle improvements via education programs.
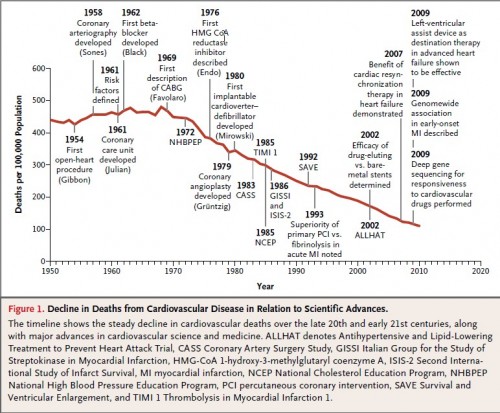
For these efforts, we have been rewarded with dramatic reduction in cardiovascular disease specific mortality. This chart, from the Nabel and Braunwald paper, illustrates:
A more detailed timeline of milestones in cardiovascular disease is found in a supplementary appendix (pdf). (The chart does not prove causality. Other factors may have contributed to mortality decline.)
For all that, heart disease remains one of the top causes of death in the US and “cardiovascular disease, including heart disease and stroke, is the leading cause of death worldwide, including low-income and middle-income countries.”
The experience with cardiovascular disease illustrates evidence-based medicine at its best or, at least, closer to “best” than is achieved in much of medical science. Unfortunately, not all of medicine has undergone similar, decades long scrutiny and improvement with sound scientific and public health methods. It’s well known that there is far too much eminence-based medicine,* driven by the anecdote or intuition of powerful physicians and medical groups operating under perverse incentives and within a fractured health system. We can do so much better. Our experience with cardiovascular disease proves it.
* My source for the brilliant “eminence-based medicine” is Ashish Jha.
AF