The best paper I’ve read documenting the various inefficiencies of the US health system is this, ungated PDF, by Katherine Baicker and Amitabh Chandra. Since it is ungated and fairly accessible, I’m not going to unpack it. You can read Jeff Levin-Scherz’s summary at the Managing Healthcare Costs blog, but I really think it is worth your time to read the whole paper. It’s that good.
I want to zero in on one point they make. Actually, they make it several times and it’s the main point of the paper:
- “We are neither allocating resources efficiently between health and other uses, nor getting as much health as we could for every dollar spent – making it difficult to evaluate how much we ‘should’ be spending on health care.”
- “It is in fact impossible to evaluate allocative inefficiency in the presence of productive inefficiency.”
- “Different policy levers operate on different sources of inefficiency, and allocative efficiency cannot be evaluated when productive inefficiency persists.”
The distinction between allocative and productive efficiency is crucial to policy, so I think it’s worth understanding. In their words,
Productive efficiency [means] that health care resources are put to the best use possible and produce as much health as they can, and allocative efficiency [means] that the right share of resources is being devoted to health care versus other goods in the economy.
Put another way, allocative efficiency pertains to whether we’re spending the right amount on health care in general, which today comes to about $2.75 trillion or 17.8% of the US economy. Productive efficiency pertains to whether we’re using those resources devoted to health care most efficiently. I find the easiest way to understand this graphically is to consider a chart from another paper by Chandra and colleagues, about which I wrote before.
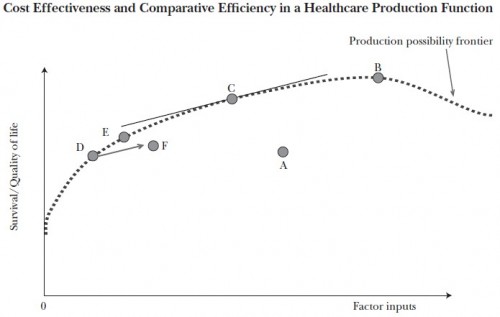
Allocative efficiency pertains to selecting the right “factor inputs” (dollars) to devote to the health system. Productive efficiency is about maximizing the value obtained for those dollars, or operating on the production possibility frontier. Baicker’s and Chandra’s point is that you can’t achieve allocative efficiency without productive efficiency. To see why, consider point A in the chart. There is no way to argue that the factor inputs corresponding to point A are allocatively efficient. After all, one could achieve the same output (survival/quality of life) as obtained at point A for far fewer resources. Point D does so. In moving from point A to D, resources are freed up that were not necessary to provide the level of health and benefit. Those resources could go to other goods or services that do provide value. Thus, A cannot be allocatively efficient precisely because it is not productively efficient.
Just because the system is operating on the production possibility frontier does not mean the operating point is allocativley efficient, though it is productively efficient from the vertical axis up to point B. (After point B one can obtain the same quality with fewer resources.) My prior post about this chart explains how point C is allocatively efficient because it meets society’s (somehow and hypothetically) agreed upon level of marginal quality of life per factor input or QALY/cost. The other points on the curve (up to B), though productively efficient, are not allocatively efficient for this reason. Productive efficiency is a necessary but not sufficient condition for allocative efficiency.
Now, the policy connection: The very fact that the health system cannot be using an allocatively efficient level of resources without first being productively efficient means we should place a higher priority on the latter than the former. That means instead of devoting our time, energy, and political capital on the level of health spending, we should devote it to producing health more efficiently. Yet, we seem to largely do the opposite. Far more attention is given to how much we spend on health care than how to make that spending more efficient. Often, when the latter is brought up, it’s shouted down as “rationing.” If “rationing” means “productively efficient” we should embrace the term.
Studies of effectiveness of health interventions are not rationing. Moreover, they’re essential. If one cares about allocating the right level of resources to health, one has to first move the system toward productive efficiency. Baicker and Chandra conclude,
Perhaps the most important contribution that public policy could make to system-wide efficiency would be to generate more information – for both patients and providers – about what care is in fact high value. […]
Because such information is a public good, it is underprovided by the market, and that suggests a role for government subsidization of trials. […] Improving our knowledge of what works is a prerequisite for increasing productive efficiency and eliminating medical practices that are unsafe at any price or dominated by other treatments. […]
By first ensuring that health care resources are used more productively, we will be in a much better position to move towards spending the “right” amount on health.
Comparative effectiveness research must come before we can conclude what is the right amount to spend on health care. Moving resources from those that have lavish health insurance and the health care it affords to those that do not is also a step toward productive efficiency, though is far from the only necessary one. Hence, this is an argument for achieving universal coverage or access to productive care before attempting to deduce the right amount to allocate to the health sector.
AF