In JAMA Internal Medicine, David Levine, Jeffrey Linder, and Bruce Landon look at progress in improving quality of care in the US since 2002. They are not impressed.
Objective. To measure changes in outpatient quality and patient experience in the United States from 2002 to 2013.
Design, Setting, and Participants. We analyzed temporal trends from 2002 to 2013 using quality measures constructed from the Medical Expenditure Panel Survey (MEPS), a nationally representative annual survey of the US population… Participants were noninstitutionalized US adults 18 years or older (range, 20,679-26,509 individuals each year).
Measures. Outpatient quality measures were compiled through a structured review of prior studies and measures endorsed by national organizations. Nine clinical quality composites (5 “underuse” composites, eg, recommended medical treatment; 4 “overuse” composites, eg, avoidance of inappropriate imaging) based on 39 quality measures; an overall patient experience rating; and 2 patient experience composites (physician communication and access) based on 6 measures.
The authors acknowledge that there are limits to how well you can measure the quality of care with these methods. Nevertheless, if quality of care was improving quickly, that change should be reflected even in these imperfect measures. Was it?
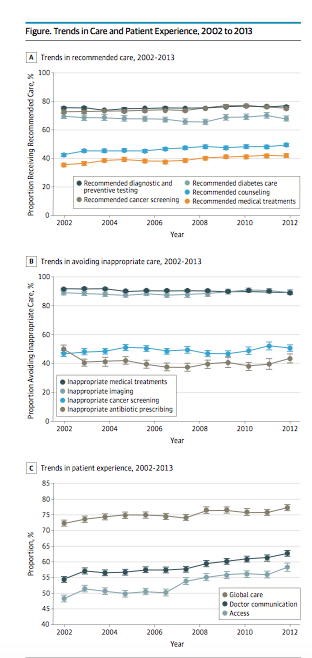
Results. From 2002 to 2013 (MEPS sample size, 20,679-26,509), 4 clinical quality composites improved: recommended medical treatment (from 36% to 42%; P < .01), recommended counseling (from 43% to 50%; P < .01), recommended cancer screening (from 73% to 75%; P < .01), and avoidance of inappropriate cancer screening (from 47% to 51%; P = .02). Two clinical quality composites worsened: avoidance of inappropriate medical treatments (from 92% to 89%) and avoidance of inappropriate antibiotic use (from 50% to 44%; P < .01 for both comparisons). Three clinical quality measures were unchanged: recommended diagnostic and preventive testing (76%), recommended diabetes care (68%), and inappropriate imaging avoidance (90%). The proportion of participants highly rating their care experience improved for overall care (from 72% to 77%), physician communication (from 55% to 63%), and access to care (from 48% to 58%; P < .01 for all comparisons).
Levine et al. conclude:
Despite more than a decade of efforts to improve the quality of health care in the United States, the quality of outpatient care delivered to adults has not consistently improved. There have been improvements in patient experience. Current deficits in care continue to pose serious hazards to the health of the American public in the form of missed care opportunities as well as waste and potential harm from overuse.
So why has progress been so slow? In 2003, Elizabeth McGlynn and several colleagues published an important benchmark documenting quality problems in US health care. McGlynn, John Adams, and Eve Kerr have a commentary on Levine et al. in the same issue of JAMA Internal Medicine. They argue that
Much of the work in quality improvement has focused on approaches that are driven by payers and policy makers. These have included measurement and public reporting, payment incentives, investments in electronic medical records, and developing virtual systems of care in select areas. None of these approaches by itself is likely to fundamentally alter the level of quality delivered throughout the nation. To do so requires significant work by health professionals on the front lines in collaboration with their patients. And those approaches require time, resources, and energy that are beyond what is available to many practices that are struggling to keep up with a rapidly changing world.
I strongly agree that:
- Measurement in and of itself does little,
- Incentives won’t always change behaviour, particularly if the cost of change outweighs the value of the incentive, and
- Quality improvement is accomplished by “health professionals on the front lines in collaboration with their patients”.
But I don’t think these points quite capture why it’s so hard to improve medical quality. I see two reasons why we might have expected change to be faster. First, we expected change to be fast because we looked at dramatic improvements in quality achieved in other industries, such as automobile manufacturing. Second, other nations deliver care that looks at least as good (or better) than US care, at significantly lower cost. This makes it seem like that there should be low-hanging fruit to harvest, that is, we should be able to make quick changes that move us to a higher quality of care without increasing cost.
Change is hard, in my view, because the fruit is harder to pick than we thought. The fruit is hard to pick in part because delivering health care is not much like making a car.

Auto manufacturing involves highly standardized and intensively automated workflows. Changing how work gets done may require a lot of capital investment. Nevertheless, a numerically-controlled lathe will change what it does when you reprogram it. And you don’t need to worry about the expectations of the steel that the lathe shapes. Medical work is much less standardized. No two patients are the same, biologically, psychologically, or in their social circumstances. Unlike steel, patients have agency that the care system should and must accommodate. All this makes caregiving a matter of craft skills, and care ‘algorithms’ are often more like suggestions. Above all, because they are craftsmen and craftswomen, and not robots, caregivers can be nudged, but they can’t be programmed.
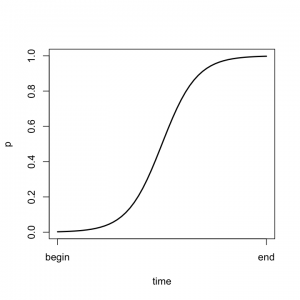
The point is not that changing medical practice is impossible, but rather that it is hard and slow. There is a an old model in the theory of diffusion of innovations that argues that the adoption of a new idea or practice follows an S-shaped (logistic) curve. In the graph to the left, the vertical axis is the proportion of enterprises that use a new idea. Initially, and for a considerable time, adoption is slow, because early adopters have to work out the kinks, overcome poltical resistance to the new idea, and so on. When these problems get solved, change is easier, and adoption speeds up.
My hope is that the problem is that improvement in the quality of health care is slow because we are still on the left hand side of the curve, and change will speed up in the future. Or, perhaps, we will eventually figure out how medical care can be automated.

