Aaron’s recent posts on waiting times in the US and Canada (and Austin’s prodding) have convinced me to add a little more data to the conversation. Julia Prentice and I did a study of the effect of waiting times on mortality among elderly American veterans who use VA outpatient geriatric clinics. VA medical centers offer low-cost or free medical care to qualifying veterans, so demand for care typically exceeds the available supply by a larger margin than in most of the US system. We studied these particular patients because the VA has electronic waiting times data and because these patients had numerous health conditions that we thought would make them vulnerable to bad outcomes if they had to wait for care.
The key figure, shown below, illustrates that risk-adjusted mortality rates increased with waiting times, but the relationship was not as strong as some might expect. The risk of mortality increased about 20% starting at an average wait time of 31 days (the increases at the far right and far left of the figure were not significant because of sparse data).
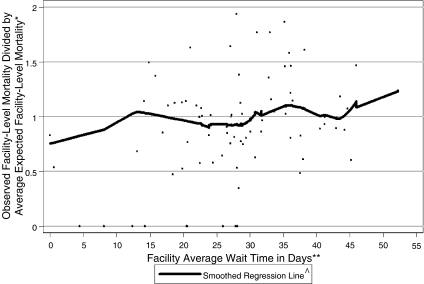
I should emphasize that the waiting times in this study were for all outpatient encounters with physicians, not just elective surgery, which is often the subject of comparisons between the US and Canada. Still, there’s evidence that waiting for care is bad for you, particularly if your health is fragile and the waits for appointments are in excess of 30 days.

