One of the persistent misunderstandings of mental illness was — unfortunately — perfectly expressed in a recent Slate Magazine article. Discussing the Oregon Medicaid Experiment, the headline writer stated that
One of the persistent misunderstandings of mental illness was — unfortunately — perfectly expressed in a recent Slate Magazine article. Discussing the Oregon Medicaid Experiment, the headline writer stated that
A new study suggests universal health care makes people happier but not healthier.
Apparently the writer believes that ‘Health’ = ‘Physical Health,’ whereas ‘Mental Health’ = ‘Subjective Well-Being.’ This misunderstanding promotes views that physical illness is real and must be treated, whereas the mentally ill… well, they need to suck it up.
It’s true that unlike mental illnesses, some physical illnesses kill you directly by stopping your breathing or your heart. But if you look at the data (for example, here or here) you find that the mentally ill die a lot earlier than those who do not have mental illnesses.
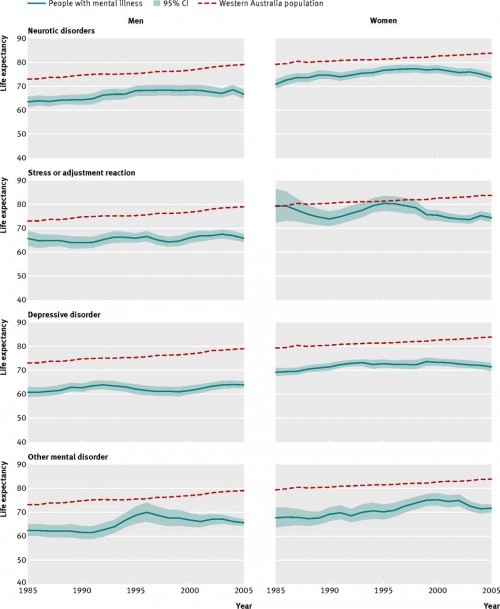
The figure below is from a recent paper in the BMJ by David Lawrence, Kirsten Hancock, and Stephen Kisely. The horizontal axis in each graph is historical time, the vertical axis is life expectancy. The red dotted line is the average life expectancy of Western Australians from 1985 to 2005. The blue line is the life expectancy of mentally ill Western Australians.
Lawrence et al found that, first, mental illness is associated with a substantial life expectancy loss and, second, this loss is increasing over time.
the size of the gap in life expectancy for people with psychiatric disorders in Western Australia increased between 1985 and 2005, from 13.5 to 15.9 years for males and from 10.4 to 12.0 years for females.
This is big: The mortality difference associated with having a mental illness is comparable to that associated with being a life-long smoker. The reason the gap is growing is that life expectancy is improving among the non-mentally ill but not much among the mentally ill.
So mental illness isn’t just about happiness: Mental illness kills. Sometimes by suicide, of which mental illness is a principal cause. But most of the excess deaths among the mentally ill are caused by diseases such as cardiovascular disease or cancer. In a sense, mental illness amplifies the risk or lethality of physical health problems. This occurs for many reasons. Mentally ill people are more likely to develop tobacco, alcohol, and substance abuse addictions. Mentally ill people also experience high levels of stress from the loss of jobs, marriages, and families. Chronic diseases such as diabetes require intensive daily self-care routines and mental illness undermines a patient’s ability to carry these out.
The causal story relating mental and physical illness is complex. Each may promote the other and both kinds of illness are promoted by stress and other social determinants of health.
The essential point, however, is that it is a terrible mistake to equate “health” with “physical health.” The unity of the body and mind is not just new age rhetoric. It also points to the comprehensive physical suffering of the mentally ill.
@Bill_Gardner