Background
The days and weeks after being in the hospital are a vulnerable period, sometimes followed by readmission. High hospital readmission rates in an area can be influenced by factors like socioeconomic status or lack of community support systems. Health system-related failures can also contribute to patient readmission. For instance, gaps in post-discharge care, poor home or nursing home care management, or receiving care at low-quality hospitals can all lead to higher 30-day readmission rates. Ongoing research highlights the importance of addressing social and health system disparities to lower readmission rates.
New research
Evaluators at the Partnered Evidence-based Policy Resource Center (PEPReC) and other partner institutions added to this body of literature in a recent paper by investigating the relationship between the local supply of post-discharge care options and hospital readmission rates for patients with acute myocardial infarction (i.e., heart attack), heart failure, or pneumonia.
Study Methods and Limitations
The authors consolidated data (2013-2019) from the Centers for Medicare and Medicaid Services, the American Hospital Association, the Census Bureau, and the Health Resources and Services Administration. Once condensed, the sample was generally reflective of American hospitals, with over 50,500 hospital-condition-years from over 3,000 unique hospitals included.
Controlling for hospital characteristics, patient demographics, and clinical factors, the authors used multivariable regression models to isolate the impact of local post-discharge care supply on hospital readmission rates. The authors conducted analyses with all three health conditions pooled together as well as with each condition individually.
There were some limitations to the study. For instance, the authors relied on secondary data and could not identify specific reasons why certain post-discharge care options generate more readmissions. Additionally, the data did not differentiate which readmissions were potentially preventable through improved quality of care.
Findings
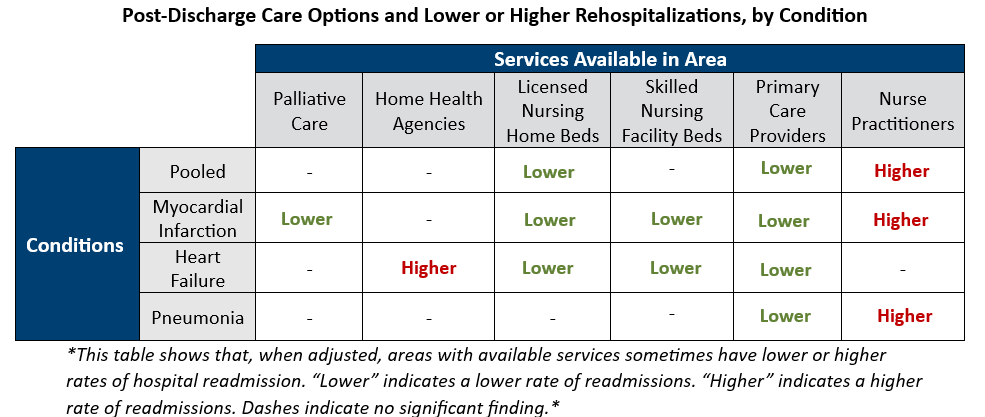
From 2013 to 2019, the population-level availability of post-discharge care options varied greatly by county. When controlling for differences in hospital characteristics, patient demographics, and clinical factors, hospitals in areas with more primary care doctors and nursing home beds had lower readmission rates. Hospitals in areas with greater availability of palliative care and skilled nursing facility beds also had reduced readmissions, though only for individual conditions and not when the three conditions were pooled.
On the other end, hospitals in areas with more available home health agency services saw higher readmission rates for patients with heart failure. Similarly, when conditions are pooled or when analyzing only heart failure or pneumonia, areas with more nurse practitioners are found to have increased readmissions. The authors pointed out that home health agencies experience frequent staffing changes, and areas with higher levels of nurse staffing tend to have greater patient acuity, which may explain these findings.
The figure below represents the findings visually.
Conclusion
After reviewing their findings, the authors argued that improving continuity of care for patients post-discharge would improve patient outcomes. They also proposed that the federal system designed to fine hospitals for high readmissions rates should consider these local health system characteristics to more accurately assign penalties.
Returning to the hospital after recently being discharged isn’t an experience most people want. It’s costly and inefficient. This study speaks to the importance of the availability of post-discharge care services to prevent that experience, offering policymakers a better way forward.
PEPReC, within the Veterans Health Administration and funded in large part by the Quality Enhancement Research Initiative (QUERI), is a team of health economists, health services and public health researchers, statistical programmers, and policy analysts who support VA efforts to improve Veterans’ lives through evidence-driven innovations using advanced quantitative methods.

