… a research notebook entry.
From Predicting time to readmission in patients with recent histories of recurrent psychiatric hospitalization: a matched-control survival analysis, by Schmutte, Dunn, and Sledge:
Reducing readmission rates among adults with histories of frequent hospitalizations remains challenging (Gerolamo, 2004; Montgomery and Kirkpatrick, 2002); however, a recent study did find that for adults with schizophrenia and histories of frequent inpatient stays (i.e., 4 or more previous hospitalizations), receipt of outpatient aftercare interventions that focused on symptom education, care continuity, and daily structure was associated with fewer readmissions within 3 months (Prince, 2006). On the other hand, there is evidence that helping patients find and maintain employment is associated with reduced hospitalizations (Burns et al., 2009; Drake et al., 1996; Henry et al., 2004). […]
Despite multiple clinical and demographic differences between adults with and without recent histories of recurrent hospitalizations at the time of index hospitalization, only unemployment and living in supervised residential living facilities predicted shorter time-to-readmission within 12 months of hospital discharge after controlling for prior hospitalizations. Unemployment and residential living status were not associated with psychosis or moderated by illness severity or comorbid substance use. These results suggest that early psychiatric readmission may be more influenced by residential and employment status than by severe mental illness.
From Predictors of Rehospitalization in High-Utilizing Patients in the VA Psychiatric Medical System, by Bowersox, Saunders, and Berger:
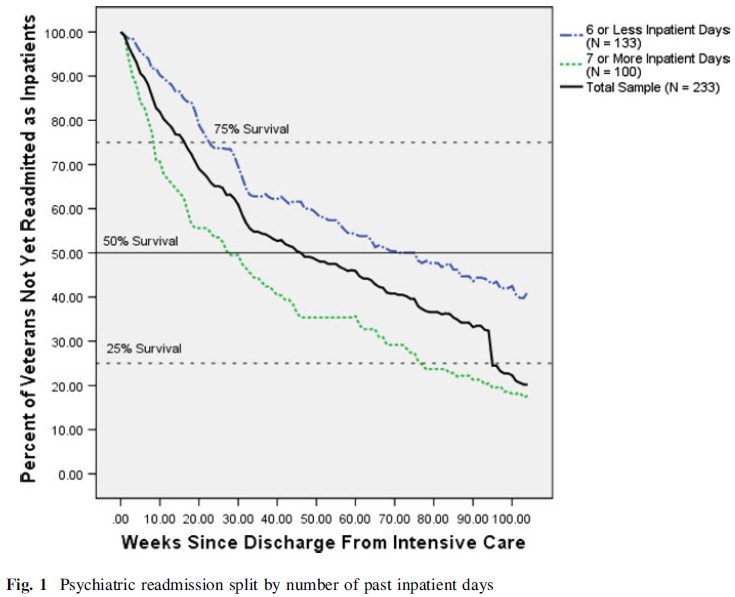
One consistent finding is the relationship between past inpatient psychiatric admission and future readmission, with patients who have received inpatient care in the past being more likely to be readmitted for future inpatient care [6, 7]. Investigation into other factors such as self-reported patient symptoms [8] and diagnosis [3, 9] have yielded inconsistent results, causing some researchers to suggest that future approaches to this question should focus on treatment-related factors such as treatment adherence and continuity of care rather than demographic or clinical characteristics alone [10]. […]
The lack of any significant relationships between short-term treatment engagement and later hospitalization is noteworthy, as this relationship has been found in several previous investigations into this area [2, 32]. Similarly, the lack of relationships between treatment cognitions and readmission is a concern as the presence of such a relationship would allow for the development of interventions aimed at the reduction of readmission. Further, the absence of any relationship between readmission and diagnosis suggests that there are likely several pathways to readmission, with different patients requiring emergency-level services based on different symptoms and circumstances.
From Suicide Risk and Acute Psychiatric Readmissions: A Prospective Cohort Study, by Mellesdal et al.:
Some cohort- and register-based studies that focused on psychiatric diagnoses as possible predictors of psychiatric readmission found increased readmission rates to be associated with a diagnosis of psychosis or personality disorder (6) or an affective disorder (7). Co-occurring disorders, in particular a substance use disorder and schizophrenia, have been found in some studies (8,9) but not in others (7) to increase the risk of readmission. […]
Fifty-four percent of the total admissions and 62% of the readmissions in this [Norwegian] patient sample were related to suicide risk. Furthermore, patients with more readmissions were more likely to be readmitted for suicide risk. Patients with an index admission related to suicidal ideation or planning had increased risk of readmission because of suicide risk. A history of psychiatric hospitalization during the previous year, having a personality disorder or a substance use disorder, and living alone or receiving a disability pension or social or unemployment benefit also predicted readmission.
From Effectiveness of Peer Support in Reducing Readmissions of Persons With Multiple Psychiatric Hospitalizations, by Sledge et al.:
Objective: The study examined the feasibility and effectiveness of using peer support to reduce recurrent psychiatric hospitalizations.
Methods: A randomized controlled design was used, with follow-up at nine months after an index discharge from an academically affiliated psychiatric hospital. Patients were 18 years or older with major mental illness and had been hospitalized three or more times in the prior 18 months. Seventy-four patients were recruited, randomly assigned to usual care (N=36) or to a peer mentor plus usual care (N=38), and assessed at nine months.
Results: Participants who were assigned a peer mentor had significantly fewer rehospitalizations (.89±1.35 versus 1.53±1.54; p=.042 [one-tailed]) and fewer hospital days (10.08±17.31 versus 19.08±21.63 days; p<.03, [one tailed]).
Conclusions: Despite the study’s limitations, findings suggest that use of peer mentors is a promising intervention for reducing recurrent psychiatric hospitalizations for patients at risk of readmission.