The world is in the grip of two simultaneous disasters: the COVID-19 pandemic and a shocking fall in economic activity. In response to the first, many countries have closed businesses and ordered their citizens to stay at home. This whole or partial lockdown is one cause of the fall in the economy. So there is a tradeoff: the longer we are in lockdown, the deeper the recession, and conversely. This has led to a heated debate about when we should end the lockdown and return to work.
In this post, I argue that the question ‘when do we return to work’ is too simple. We should be discussing not when but when and how we should return to work. By ‘how’ I mean, do we return to the status quo before the pandemic, stepping back into the lives we led before? Or, as we return, do we change how we live to reduce the threat of the pathogen? If the latter, what specific changes are needed?† I am going to focus on just the how, not the when, and on only one aspect of how: How can we return from work while protecting the elderly and sick from COVID-19?
David L. Katz of the Yale School of Medicine has a plan for when and how we should return to work. This plan has been championed by Tom Friedman and many other pundits. In essence, we should sustain the lockdown for a brief period to reduce the risk of overwhelming the health care system with severe COVID-19 cases. However, we would not stay in lockdown until the prevalence of the virus gets so low that people can congregate with minimal fear of transmission. That would cause too much economic harm. Katz argues, therefore, that only the young and healthy would return to work.* Some returned workers would become infected with the still-prevalent coronavirus. This is acceptable, on Katz’s view, because the young and healthy have only a small risk of dying from COVID-19. Conversely, the chronically ill and the elderly are at substantially higher mortality risk. Therefore, when the young and healthy return to work, we should make special provisions to protect the elderly and chronically ill. If we succeed in protecting the vulnerable from becoming infected, we will greatly reduce the morbidity and mortality of the disease. This would give us a better tradeoff, and allow us to return to work earlier and restart the economy faster at a lower cost in lives.
Friedman quotes Katz as foreseeing only two more weeks of social distancing. Few epidemiologists regard that as sufficient. However, whether Katz is right about when to return to work is to some degree beside the point. The proposal to allow the less vulnerable young to return to work early while protecting the vulnerable is a superb idea. If it works.
It won’t work if the protections that we plan are ineffective or if we do not implement them in an adequate way. And if the protections fail while the virus is still prevalent, many elderly Americans will die.
So we need to think seriously about how we would protect vulnerable populations. There are about 52 million Americans aged 65 years or older. The CDC has identified several conditions that increase vulnerability to COVID-19. These include heart disease, moderate to severe asthma or other chronic lung diseases, being immunocompromised (including cancer treatment), having BMI ≥ 40, or having poorly controlled diabetes, kidney, or liver disease.§ Many elderly Americans have one or more of these conditions. For example, in 2010, 37.2% of Americans 65 or older reported that they had been diagnosed with heart disease.
What are the living situations of elderly Americans?
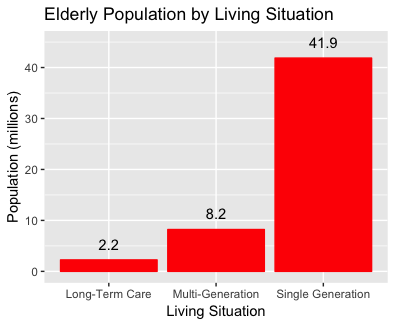
About 42 million Americans live in households only with people their own age. Some of these are in retirement communities, but most are in neighbourhoods or apartment buildings that mix older and younger people. Some proportion of these younger people will be infected and, therefore, potentially a risk to the elderly living among them. In addition, more than 8 million elderly live with their children or grandchildren; These older adults will have even more intimate contact with the young.
So how would we protect the elderly? Working or not, most elderly people will be shopping, riding elevators, and so on with younger people. Should we require every retailer, every restaurant, and every subway and airport to carry out regular disinfection protocols, the way hospitals do? If so, we need to begin to write up those plans, including plans for staff training and compliance inspections. Do we want to encourage the elderly (or everyone?) to wash their hands every time they touch another person? The history of handwashing campaigns in hospitals is not encouraging, but even partial compliance might help. Do we have a campaign ready to teach this behaviour? Should the elderly (or everyone?) routinely wear protective equipment, e.g., surgical masks? If so, we need to ensure that there is an adequate supply, that every senior gets one, and that they understand that it is essential to wear one.
There are also 2.2 million elderly Americans in long-term care. As we discussed in a previous post, this group is at extremely high risk. They are both old and have compromised health. Moreover, in long-term care, large groups of patients cohabitate in confined settings with communal meals and many group social activities. Moreover, many residents are incapable of practicing the levels of personal hygiene required to stop the transmission of the virus. Disease outbreaks are common. All the safety procedures discussed above would need to be practiced in this setting, and then some. There are 15,600 licensed nursing homes 28,900 licensed residential care centers, so implementing protective policies in this sector will be a serious hassle. There are also a large number of unlicensed facilities. Licensed long-term care facilities employ about 1.25 million staff, but that number would need to be increased to ensure adequate implementation of infection control, increasing the cost of an already expensive service.
Bottom line, if we leave lockdown before the virus is fully suppressed, then protecting elderly Americans will require a costly and demanding effort. Moreover, the effectiveness of the protective measures that I have discussed is uncertain. ‘Strategies’ for return to work that do not include detailed plans for protecting the vulnerable are just handwaving. The proposal that we could organize meaningful protection for the elderly in the next two weeks is wishful thinking. Returning to work sometime before the complete suppression of the coronavirus may nevertheless be the tradeoff that society wants to make. But if we want to do it while protecting our elderly, we need to begin serious planning and mobilization of resources now.
†I am not going to discuss the role of testing here. Every credible return-to-work strategy assumes that we will carry out as much testing as possible for coronavirus, with selective quarantine of those who test positive. However, this will take time to work, and it will be less effective if we return to work early when the virus is still prevalent.
*But what if the elderly want or need to work? Before the pandemic, 24% of men and about 16% of women ages 65 and older were in the labour force before the current recession hit. Do we have the legal means to exclude them? If we do exclude them, how do we make up for their income loss?
§Someone with access to the Medical Expenditure Panel Survey could do a public service by estimating how many Americans have at least one of these conditions, by age group.

