I’ve written before that I use this blog as my research notebook. Trust me, it’s an extremely valuable way to preserve my (terrible) memory of details about what I’ve read. To the extent that readers who are also subject-matter experts chime in, it can also enhance the quality of my work. If you care about the subject, this is of benefit to you (and your professional community) too because it improves my treatment of it in future posts. In case you want to play along, I’m indexing questions in each post with the notation “[Q#]” where # is an integer. These are end-notes. Scroll down and see if you can answer any of my questions, if you wish.
With that as general explanation, I’m going to be blogging some notes about prostate cancer. Some of these posts will be way, way down in the weeds and may bore the stuffing out of many readers. If you’re one of them, just move on. Note, however, that I will try to make the actual language of weedy posts humorous, because I use humor to distract from my lack of wisdom. Other posts may be at a higher level, more directly pertaining to policy or coverage decisions, so they’ll be more inherently interesting.
This one is weedy. You’ve been warned.
***
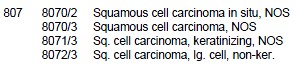
I’m beginning to get up to speed on prostate cancer morphology and data coding thereof. It appears to me as if the data standards are codified in ICD-O-3 documentation. (ICD = “international classification of diseases,” O = “oncology,” and 3 = third edition. And, yes, there is a Wikipedia page for it.) In particular, I’ve been “enjoying” the prostate cancer section of the ICD-O-3 SEER Site/Histology Validation List (pdf). (That’s ICD-O-3 topographical type C619 for those of you scoring at home.) A portion of that section looks like this:
I will confess, I barely don’t understand cancer terminology yet, so I plucked out part of the “squamous cell” chunk of codes because “squamous” has an interesting sound, though probably not to those with squamous cell cancer, whose likely challenging relationship with the word I fully acknowledge. It makes me think of someone who is squeamish about being famous. “Oh he doesn’t talk to the press. He’s squamous.” Vastly more about squamous cell cancer here, only a bit of which I’ve read as of this writing.
It’s pretty clear from the organization of the ICD-O-3 that you’ve got your topographical code (prostate = C619) and then you’ve got your “higher level” morphology code [Q1] (807 = squamous cell carcinoma). See how all the entries in the exhibit above start with “807”? But then there are two more numbers, one preceding and one following a forward slash (/). These indicate “lower level” morphology (or sub-types) [Q2]. The number immediately before the slash is an integer in sequence (0, 1, 2, 3, …). For prostate cancer, the number following the slash is always a 2 or a 3. Often, but not always, a 2 is associated with an “in situ” type, meaning, I think, that the cancer has not invaded surrounding tissue [Q3]. There are all manner words affiliated with sub-types: small, giant, clear, noninvasive, keratinizing, NOS, and some others. I don’t know what they all mean. I don’t know what makes a “/2” a “/2” and what makes a “/3” a “/3” [Q4]. I don’t know what work the slash does, though it suggests yet another level of typology (finer level after the slash) [Q5].
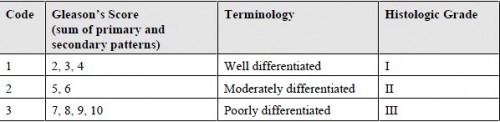
Switching gears, another bit of information of interest in my research is a prostate cancer’s Gleason score. Trouble is, some of the data I will be using doesn’t have Gleason score coded. So, I’m wondering whether I can infer it (or, if not it exactly, at least to within some range) from other information. With that in mind, I noticed the following in the 2010 edition of the Facility Oncology Registry Data Standards (FORDS) manual (pdf). (There is a 2012 FORDS manual, as well as older editions.)
Perhaps a range of Gleason score can be inferred from terminology and/or histolic grade, if the associations implied by the chart are standards that are widely followed.
I’ll stop here for now and get back to my reading.
Questions (see text)
Q1: “Higher level” is probably not the right terminology here. What is?
Q2: Again, what’s the proper terminology for these lower level codes?
Q3: Right?
Q4: Help?
Q5: Yes?