Katherine Baicker and Amitabh Chandra explored the relationships among physician workforce composition, Medicare spending, and quality in a 2004 Health Affairs article (ungated). Broadly, they found that higher spending is associated with lower quality. More interestingly, however, they suggest why: too many specialists relative to general practitioners.
This suggests that specialists are clustered in areas where costly intensive care crowds out high-quality care and that one mechanism for this is a lesser presence of general practitioners. Encouraging greater access to general practitioners, or involving specialists in the provision of effective care, could improve the overall quality of care received by elderly Americans.
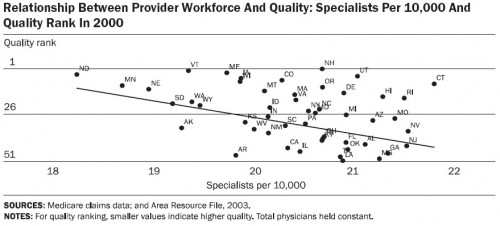
Their charts and tables tell the story. Below are four that support the quote above. First, let’s consider how state quality rank relates to physician workforce composition. And by quality rank I (they) mean the average of the ranks for the 24 quality measures developed by the Medicare Quality Improvement Organization. The more specialists per capita, the lower a state’s quality rank. (Note: for all charts, total physicians per capita is held constant.)
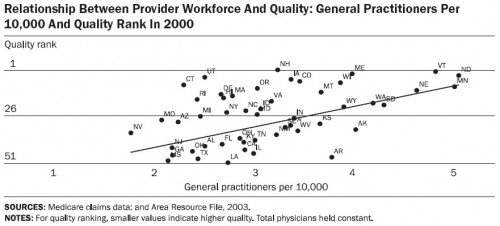
But the more general practitioners per capita, the higher the state’s quality rank.
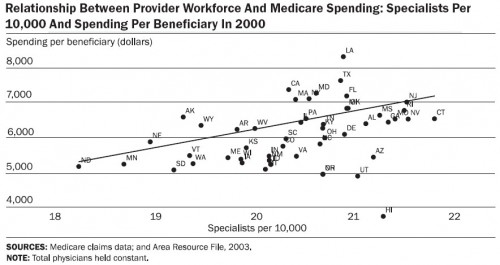
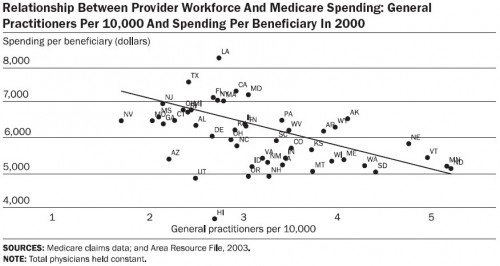
What about spending? Well, specialists cost a lot more than general practitioners. Here are the charts, first specialists and then general practitioners:
Maybe this particular quality rank is biased against specialists? The authors write,
It is possible that although areas with more specialists do not provide higher quality care along these dimensions, they may be better at the treatment of more acute conditions. It is also possible that areas “specialize” in different types of care: Some areas specialize in primary care, while others may specialize in the delivery of technologically aggressive care for heart attacks. We do not find evidence of this here: States with more specialists have neither lower mortality rates from all causes nor reduced post-AMI mortality.
Maybe the states vary so much in patient health that high spending areas need more specialists. Could be, but it likely doesn’t account for all the variation. There is even evidence that areas with greater need have fewer specialists. (See, for example, the work of David Goodman et al.) Moreover, there is no excuse for high spending areas not to deliver quality care. The quality metrics that underlie the ranks are process measures that correspond to evidence-based, effective care. Everybody should be receiving such care, and especially those with greater health risk. They should not be underprovided just because a region has more specialists.