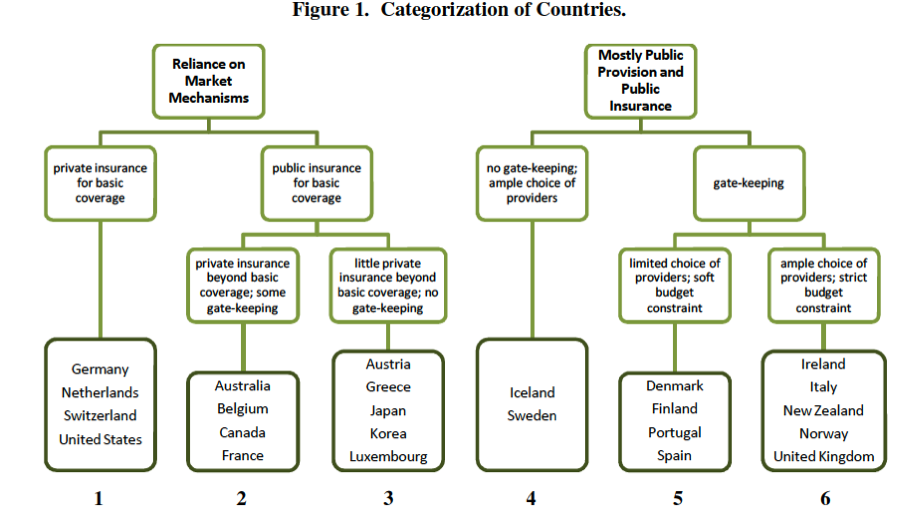
An interesting paper from Ted Ruger’s seminar at Penn Law, by Jessie Smith Nibley, looks at health outcomes across OECD countries (ssrn, free registration). Of course, you’ve seen that from Aaron before. What makes this paper novel is her method of categorizing countries by salient health system structural features:
The conclusion (emphasis added):
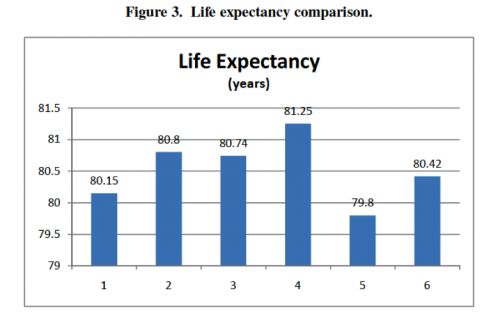
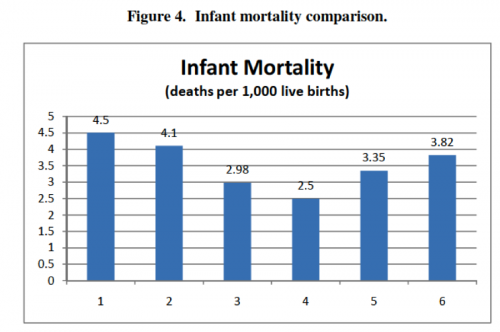
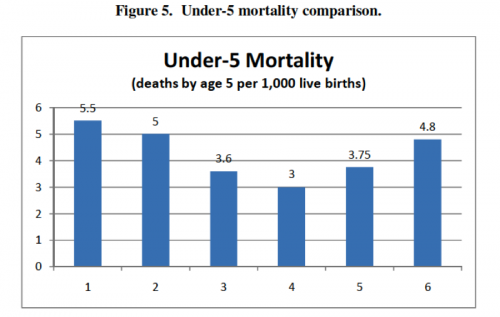
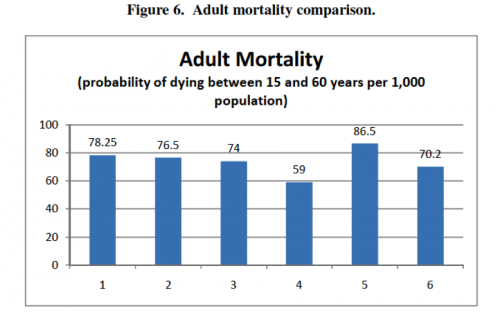
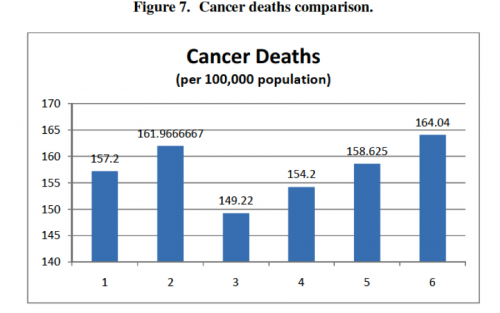
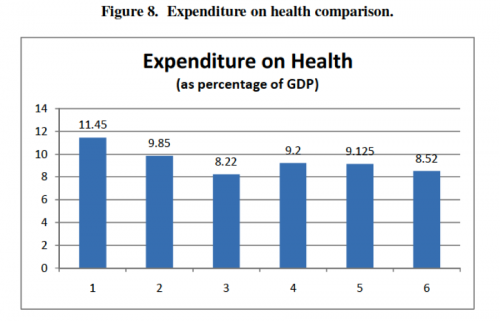
First, there is a rough bell- or upside-down-bell-curve in most of the charts—countries in the outer-most groups generally did poorly, and countries in the center groups generally performed well. In terms of the country groups’ characteristics, extremes in reliance on public or private delivery and insurance appear to be bad for health outcomes, and moderation or a mix of public and private regulation appears to be good for health outcomes. Second, Groups 3 and 4, representing countries with no gate-keeping, performed consistently well across all categories, often the best of all the groups. This trend suggests that gate-keeping may lead to relatively poor health outcomes and may be a better explanation of the curve than the extreme/moderate attributes of the groups. Finally, the high expenditure averages in Groups 1 and 2 suggest that systems based mainly on market regulation with private insurance are more expensive than mainly public systems.
Here’s the charts: