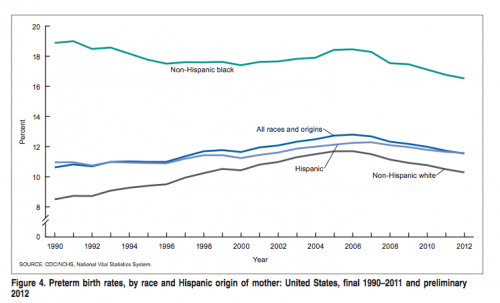
Being born very prematurely or with a very low birthweight is one of the major health risks for children, especially for African-American children. For reasons that are not fully understood (see Aaron’s discussion here), African-American women have a higher risk of delivering children prematurely.
Unfortunately, poor women in vulnerable populations often do not have an obstetrician or primary care physician from whom they can receive prenatal care. As Adrianna discussed, there are many reasons why women in vulnerable populations find it much harder to make the office visits required to get care from the primary care system.
So what should we do? Being born very prematurely is expensive and the health consequences can affect a child’s whole life. Many countries send nurses to the homes of pregnant women to ensure that they get prenatal care. But does this work?
From LeeAnne Roman, Jennifer E. Raffo, Qi Zhu, and Cristian I. Meghea in JAMA Pediatrics, there is a new and encouraging report about a program in Michigan that used home visits by nurses to deliver prenatal care.
OBJECTIVE. To test if participation in the Michigan statewide enhanced prenatal care program, the Maternal Infant Health Program (MIHP), accounting for program timing and dosage, reduced risk for low birth weight (LBW) and preterm birth, particularly among black women who are at greater risk for adverse outcomes.
DESIGN, SETTING, AND PARTICIPANTS. Quasi-experimental cohort study. Data, including birth records, Medicaid claims, and monthly program participation, were extracted from the Michigan Department of Community Health warehouse. Participants included all 60 653 pregnant women who had a Medicaid-insured singleton birth between January 1 and December 31, 2010, in Michigan. The MIHP participants were propensity score-matched with nonparticipants based on demographics, previous pregnancies, socioeconomic status, and chronic disease.
EXPOSURE. An enhanced prenatal care program.
MAIN OUTCOMES AND MEASURES. Low birthweight, very low birth weight (VLBW), preterm birth, and very preterm birth.
RESULTS. In the propensity score–matched models, black women who enrolled and were screened in the MIHP by the end of the second trimester had lower odds of VLBW (odds ratio [OR], 0.76; 95% CI, 0.59-0.97) and very preterm births (OR, 0.68; 95% CI, 0.54-0.85) than matched nonparticipants. Black MIHP participants who enrolled and were screened in the program by the second trimester and had at least 3 additional prenatal MIHP contacts had lower odds of LBW (OR, 0.76; 95% CI, 0.65-0.89), VLBW (0.42; 0.30-0.61), preterm birth (0.71; 0.61-0.83), and very preterm birth (0.41; 0.30-0.57) compared with matched nonparticipants. The MIHP participants of other races and ethnicities who enrolled and were screened in the program by the second trimester and had at least 3 additional prenatal MIHP contacts had lower odds of LBW (OR, 0.78; 95% CI, 0.66-0.93), VLBW (0.38; 0.22-0.66), preterm birth (0.77; 0.66-0.89), and very preterm birth (0.63; 0.43-0.91) compared with matched nonparticipants.
CONCLUSIONS AND RELEVANCE Participation in MIHP reduced the risk for adverse birth outcomes in a diverse, disadvantaged population. The study adds to the evidence base for enhanced prenatal care home visiting programs and informs state and federal investments.