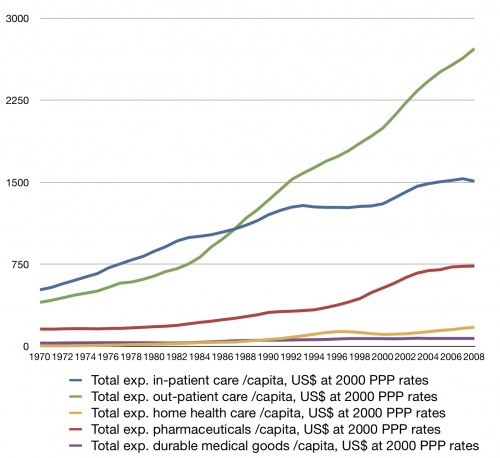
Cost chart week continues. I’ve posted graphs with outpatient and inpatient care, but people want more. So here are more data on how US spending has changed in a number of areas over the last few decades (all in US$ at 2000 PPP rates):
I’ve added expenditures on home health care (yellow), pharmaceuticals and other non-durable goods (red), and durable goods (purple).
One of these things is not like the other. For the most part, growth was consistent for inpatient and outpatient care until the 1980s. Growth in the other sectors was much slower. Starting in the early 80’s, though, outpatient care takes off in a much different way than other areas. Outpatient spending increased in the 90’s even when other areas flattened. By 2000, drug spending took off too.
One argument is that outpatient growth is due to a massive shift from inpatient care. We do know there was a shift in surgical setting in the 1980s and 1990s. I’m not seeing a very large reduction in inpatient spending though. Yes, inpatient spending slowed slightly when outpatient care took off, but not enough to compensate for the steep green line there. To argue for a huge shift in volume from inpatient to outpatient, one would have to also find a big increase in inpatient prices to keep total inpatient costs growing at nearly the same rate. Is there evidence for large increases in inpatient prices in the 1980s?
Inpatient prices paid by private plans did go up in the late 1980s as Medicare’s prospective payment system phased in (this was the golden era of cost shifting). This wouldn’t explain the early 1980s though. All in all, it seems that there was probably an increase in outpatient volume that did not substitute for inpatient care. I have no good answer as to why this would have occurred at that specific time and not before. Did something happen in the organization, politics, and economics of medical care in the US in or just preceding 1982? Was there some other change? Someone ought to know.