Among the unsurprising and uninspired provisions in yesterday’s ACA “replacement” proposal, you’ll find a predictable nod to tort reform as a means of spending control.
Let’s not mince words: defensive medicine inflates health spending, but tort reform is a snake oil cure. We know that physicians with higher malpractice premiums behave pretty much the same as those with lower malpractice premiums. We know that the GOP proposal mirrors malpractice reforms in Texas—reforms that had no meaningful impact. Ditto for California. We know that our system builds in economic incentives for providers to over-treat, independent of litigation concerns.
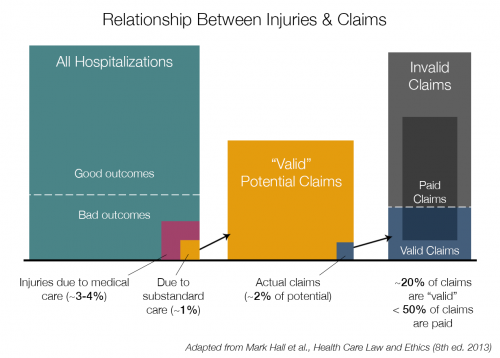
What’s more: malpractice claims are incredibly uncommon. From the universe of people who could bring valid complaints of negligence, only two percent do; only a fraction of those result in payment, often through settlement. The chart below is adapted from a legal casebook (I tweeted a photo of the original here).
That last bar might be a little confusing: only about 2% of patients who suffer negligence bring claims; they make up the blue area on the right. They’re outnumbered by claims that are frivolous or of uncertain merit (the gray area). Still, that means the number of claims filed is about 10% of what we’d see if every legitimately injured patient filed suit. And fewer than half of filed claims are paid—our current tort system sees malpractice payment for <0.05% of hospitalizations when 1% of hospitalizations could theoretically foster valid complaints.
The relevant casebook excerpt:
In any medical encounter, there is a considerable chance of a disappointing outcome. However, most of these poor results are the unavoidable consequence of the disease itself and the inherent limits of medical science. Of all hospital admissions, only about 4 percent involve an injury caused by medical treatment. Of these, only about one-fourth (1 percent of the total) are the result of substandard care. Only about 2 percent of negligent injuries result in claims being filed with insurers. In part, this is because the great majority of these injuries are temporary or minor. Importantly, however, most claims are for injuries not caused by negligence.
Some interesting evidence suggests that we could actually alter physician behavior if states changed “standard of care” laws to reflect national norms instead of “local” norms (read Nick Bagley’s take on that). That’s something I’d be interested in seeing more of, but it has to take place at the state level.
The GOP proposal—capping damages, restricting attorney fees—is small ball, because malpractice litigation isn’t as big a problem as it’s perceived to be.
Adrianna (@onceuponA)