Yesterday I wrote about a study of emergency department visits within 30 days of a surgical procedure. Last night NEJM published a study, by Thomas Tsai and colleagues, on 30-day hospital readmissons after surgery. This surgery focus is motivated by the fact that the Medicare program is considering including imposing penalties on hospitals with high surgical readmission rates.
The investigators examined 2009-2010 Medicare data for patients who had received one of the following surgical procedures: coronary-artery bypass grafting (CABG), pulmonary lobectomy, endovascular repair of abdominal aortic aneurysm, open repair of abdominal aortic aneurysm, colectomy, and hip replacement.
The paper is packed with findings. In brief, from the abstract:
The median risk-adjusted composite readmission rate at 30 days was 13.1% (interquartile range, 9.9 to 17.1). In a multivariate model adjusting for hospital characteristics, we found that hospitals in the highest quartile for surgical volume had a significantly lower composite readmission rate than hospitals in the lowest quartile (12.7% vs. 16.8%, P<0.001), and hospitals with the lowest surgical mortality rates had a significantly lower readmission rate than hospitals with the highest mortality rates (13.3% vs. 14.2%, P<0.001). High adherence to reported surgical process measures was only marginally associated with reduced readmission rates (highest quartile vs. lowest quartile, 13.1% vs. 13.6%; P=0.02).
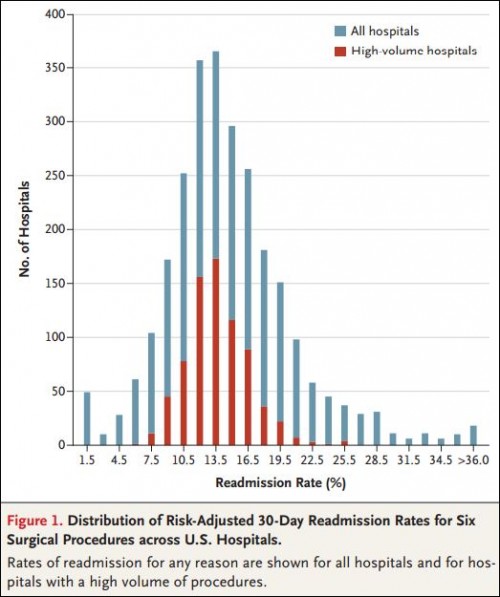
So, hospitals with higher volume, lower mortality rates, and better surgical process measures (all traditional indicators of quality) had lower readmission rates. With respect to the volume findings, here’s a pretty picture:
As readers might recall, hospital readmission rates for heart attacks, heart failure, and pneumonia are not as strongly aligned with mortality rates and other measures of quality. So, why the difference for surgical readmission rates? Tsai et al. explain:
The reasons that bring surgical patients back to the hospital soon after discharge are probably different from those that bring medical patients back. Whereas medical patients may come back because of poor social support at home, inability to access primary care, or general poor health, surgical patients are more likely to return as a consequence of complications arising from the surgery.
In other words, surgical readmission rates more closely measure hospital (surgical) quality, as opposed to the nature of care beyond hospital walls. That being the case, it makes sense that they’d be more highly correlated with other measures of hospital (surgical) quality.