The latest report from the Center for Studying Health System Change (PDF) is worth a read. What I found most informative about it–due to the nature of and deficiencies in my own base of knowledge about various topics covered–is how hospitals and physicians are paid.
The report tells us that the vast majority of physicians are paid by private plans using the same methodology as Medicare, the Medicare physician fee schedule. (We’ll be hearing a lot more about that as Congress struggles with another “doc fix” over the next month or so. The fact that it is the dominant payment method for both public and private payers makes it and its problems very important.)
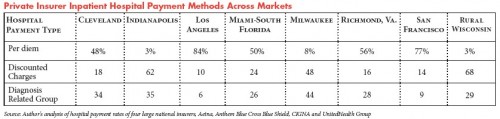
However, the report also tells us that insurers (or the largest four at least) do not use Medicare methodology, the diagnosis-related groups (DRG) system, in making payments to hospitals. Here’s the table from the report (click to enlarge):
The “per diem” and “discounted charges” methods are much more common than DRG-based payments. What does this mean? Actually, I don’t know. I know what DRGs are (more here). I can guess what “per diem” and “discounted charges” mean but my guesses don’t really help me understand how they differ or how they work and why hospitals and/or plans might prefer them to the DRG system. Can anyone help me out? Can you explain how these payment systems work or point to a good resource that does so?