I don’t have a sunny nature. That’s me to the right, at the beach with my dog. I recently shared my despair at the failure of an effectiveness trial of patient self-management.
I don’t have a sunny nature. That’s me to the right, at the beach with my dog. I recently shared my despair at the failure of an effectiveness trial of patient self-management.
But today I bring tidings of great joy to all peoples. This week’s JAMA has two encouraging randomized clinical trials of home health care.
McDermott and her colleagues tested an intervention for peripheral artery disease (PAD), a painful circulatory problem in which narrowed arteries reduce blood flow to your limbs. Among the best things to do for PAD is to walk, but the challenge is to get patients to do it, because when you have PAD it hurts to walk.
What the investigators did was to engage PAD patients in a group that exercised together and supported each other in dealing with the pain.
Our intervention applied principles from social cognitive theory, the group dynamics literature, and research on self-regulation to motivate participants to adhere to home-based walking exercise.
PAD patients in a control group received usual care and attended weekly 60-minute group sessions in which health care professionals presented lectures on managing hypertension and other health topics.
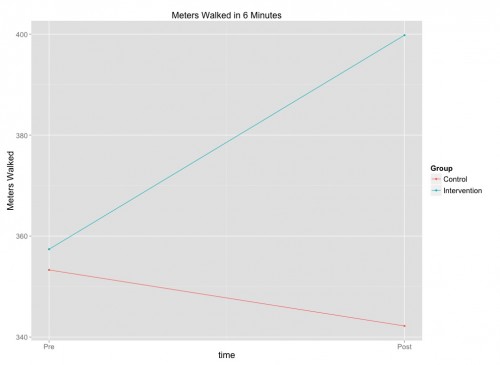
The primary outcome was the distance that patients were able to walk in 6 minutes. The control patients’ walking deteriorated from the pre-test to the post-test 6 months later (the red line below), while the intervention group improved substantially (the blue line).
The second study by Margolis and her colleagues tested a program for hypertension. Patients measured their blood pressure at home and logged it using internet-mediated telemetry. The patients then received coaching based on the data.
During the first 6 months of the intervention, patients and pharmacists met every 2 weeks via telephone until BP control was sustained for 6 weeks, and then frequency was reduced to monthly. During intervention months 7 through 12, telephone visits occurred every 2 months. After 12 months, patients discontinued use of the telemonitors, returned to the care of their primary physicians, and no longer received support from a study pharmacist.
The telemonitored and coached patients lowered blood pressure significantly more than patients in usual care, including up to 6 months after the monitors were discontinued:
Compared with the usual care group, systolic BP decreased more from baseline among patients in the telemonitoring intervention group at 6 months (−10.7 mm Hg [95% CI, −14.3 to −7.3 mm Hg]; P<.001), at 12 months (−9.7 mm Hg [95% CI, −13.4 to −6.0 mm Hg]; P<.001), and at 18 months (−6.6 mm Hg [95% CI, −10.7 to −2.5 mm Hg]; P = .004).
Cardiovascular disease is the great killer of the developed world, so any success here is wonderful news. More generally, the studies show that we are beginning to learn how to support patients in managing their chronic illnesses. To ‘manage’ a chronic disease, a patient has to change his behaviour. This sounds so easy and is so hard. The needed tools are those employed in McDermott’s and Margolis’s studies: effective home telemetry, health coaching, and patient group support.
We do not yet know how to successfully implement patient self-management support at the population scale. It will likely need the context of integrated care systems within successful accountable care organizations. But studies like these give me hope that in the next decade, we can significantly improve the effectiveness of chronic health care at an acceptable cost.