The recent paper about emergency department (ED) visits by Medicare beneficiaries within 30 days of discharge after surgery by Keith Kocher and colleagues in Health Affairs is interesting. It’s interesting for what’s in it, and it’s interesting for what’s not.
What’s in it: using 2005-2007 Medicare data, a national analysis of ED visits within 30 days of discharge for percutaneous coronary intervention, coronary artery bypass grafting, elective abdominal aortic aneurysm repair, back surgery, hip fracture repair, or colectomy.
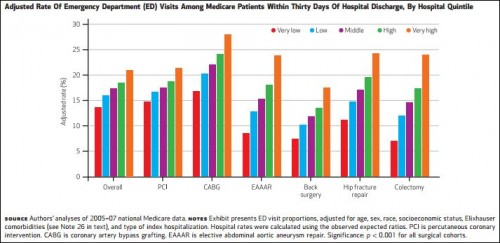
Across all procedures, 17.3 percent of patients had at least one ED visit within thirty days of hospital discharge, and 4.4 percent of patients had multiple ED visits. Among those patients who were readmitted, more than half were readmitted during an ED visit. In addition, use of the ED and related readmissions were associated with substantial variability—as much as fourfold—across hospitals.
The authors correctly point out that many such ED visits likely reflect poor coordination of care and insufficient, outpatient follow-up. They are also correct that EDs can play a role in preventing additional hospital readmissions, though unnecessary trips to the ED are bad enough. It’s also true that half of readmissions are from sources other than the ED: office, clinic, nursing home, etc.
What’s not in the paper: an analysis of 30-day follow-up ED use after discharges for conditions that are subject to Medicare’s mortality and hospital readmissions quality measures: heart attacks, heart failure, and pneumonia. Given the possibility that ED use might be serving as a substitute for readmissions, this would be a direction worth exploring. Related, it’d be nice to see the analysis conducted again for a period during which readmissions have fallen, after 2011.
This is not a criticism of the paper. I’m happy that there’s more work for researchers to do!