I’ve seen it suggested in the comments on this blog and elsewhere that low take-up rates among those eligible for Medicaid suggests they do not find the program to be of value. I have not seen any strong evidence to support that view, but I’m happy to look at it if it is suggested to me. Meanwhile, there are other potential reasons for low take-up rates including cognitive limitations.
A new study by Ifedayo Kuye, Richard Frank, and Michael McWilliams examines the relationship between cognitive limitations and awareness of and enrollment into Medicare Part D’s low-income subsidy (LIS) program, which offers reduced premiums and cost sharing for Medicare’s drug benefit to beneficiaries with incomes below 135% of the federal poverty line and assets below $6600 if single or $9910 if married (2010 figures). The investigators’ source of data was the Health and Retirement Survey (HRS). (Yes, I have switched from Medicaid to Part D’s LIS. They are different and serve different populations. Acknowledged.)
To assess overall cognitive abilities, the HRS uses a validated survey instrument modeled after the Telephone Interview for Cognitive Status, an adaptation of the Mini-Mental State Examination for use over the telephone. Participants were asked to complete a series of tasks assessing orientation, attention, memory, word recognition and comprehension, and ability to count and perform simple arithmetic. Summary cognition scores could range from 0 (no tasks completed correctly) to 35 (all tasks completed correctly).
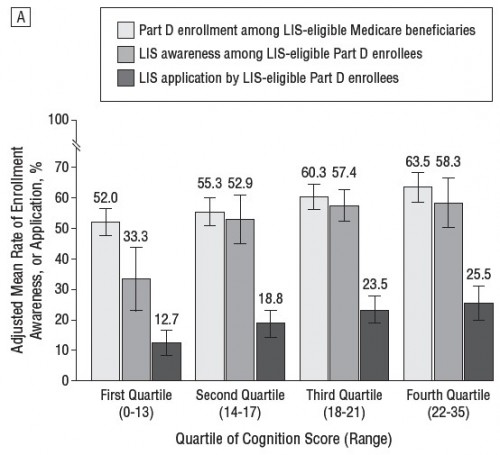
The chart below reports Part D enrollment, LIS awareness, and LIS application as a percentage of LIS-eligible beneficiaries, by quartile of cognition score. The paper includes other results by other cognitive metrics, but this suffices to make my point. Results are adjusted for age, sex, race, ethnicity, health status, chronic conditions, depressive symptoms, and difficulties with activities of daily living.
It could still be true that beneficiaries with lower cognitive skills find LIS benefits to be of less value relative to those with higher cognitive skills. Maybe the forgoing is evidence of revealed preference. This is an argument based on a market model in which consumers are reasonably, if not perfectly, well-informed about their choices. Does it seem likely to you that people with low cognitive skills are as well informed as their otherwise equivalent high cognitive skill counterparts?
Meanwhile, we have to acknowledge that only 25.5% of high cognitive skill beneficiaries eligible for the LIS enroll in it, which is just under half of those who are aware of it. Almost two-thirds of them enroll in Part D. A large proportion of beneficiaries are forgoing support for a benefit for which they are eligible and for which they are enrolled. Why? Is this revealed preference for, effectively, a lower income? Would a well-informed consumer behave that way? And these are respondents who scored high in cognition!