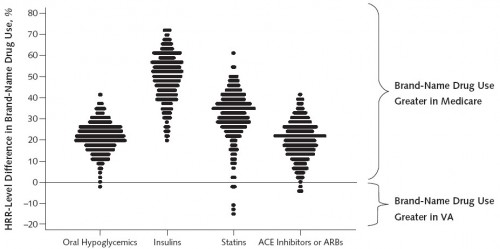
As has been documented on this blog before, VA drug prices are below those of Medicare’s Part D plans. The VA also spends less than Medicare because of a greater reliance on generic drugs, as explored in a recent study of diabetics by Walid Gellad and colleagues and for four classes of drugs: oral hypoglycemics, insulins, statins, and ACE inhibitors/ARBs.
Each dot is 1 HRR, and all HRR percentages are adjusted for sociodemographic and health status variables. More positive differences indicate higher rates of brand-name use in Medicare compared with the VA in a given HRR. Statins refer to 3-hydroxy-3-methyl coenzyme A reductase inhibitors. ACE = angiotension-converting enzyme; ARB = angiotensin-receptor blocker; HRR = hospital referral region.
The authors calculate that for these four classes of drugs, Medicare would have spent $1.4 billion less (39%) in 2008 if Part D prescribing patterns were identical to those of the VA.
It’s worth considering whether VA patients suffered due to greater generic drug use. The authors suggest not.
[N]o evidence suggests that the differences we report reflect underuse of brand-name drugs in the VA (28 –31). In fact, the VA provides a reasonable benchmark for use of generic drugs in Medicare because it performs as well or better than commercial health plans and Medicare on several measures of quality for diabetes and related conditions (28 –31).
Furthermore, strong evidence shows similar effectiveness of generic versus brand-name drugs in the classes we studied (32–35).
Note, however, that my work with Steve Pizer and Roger Feldman does find a gross reduction in consumer welfare associated with VA’s more restrictive formulary, relative to Part D plans. The potential savings from a tighter VA-like formulary are larger than this welfare reduction.
References
28. Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49:76-88.
29. Kerr EA, Gerzoff RB, Krein SL, Selby JV, Piette JD, Curb JD, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141:272-81.
30. Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:2218-27.
31. Asch SM, McGlynn EA, Hogan MM, Hayward RA, Shekelle P, Rubenstein L, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141: 938-45.
32. Horvath K, Jeitler K, Berghold A, Ebrahim SH, Gratzer TW, Plank J, et al. Long-acting insulin analogues versus NPH insulin (human isophane insulin) for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2007:CD005613.
33. Kesselheim AS, Misono AS, Lee JL, Stedman MR, Brookhart MA, Choudhry NK, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300:2514-26.
34. Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, Patwardhan MB, et al. Systematic review: comparative effectiveness of angiotensinconverting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008;148:16-29.
35. Green JB, Ross JS, Jackevicius CA, Shah ND, Krumholz HM. When choosing statin therapy: the case for generics. JAMA Intern Med. 2013;173:229- 32.