The Kaiser Family Foundation put out a handy document that explains the upcoming key changes to Medicare Advantage (MA). I’m not going to explain all of them here (see an earlier post on updates to payment rates). I’ll just highlight two things I learned from the Kaiser issue brief.
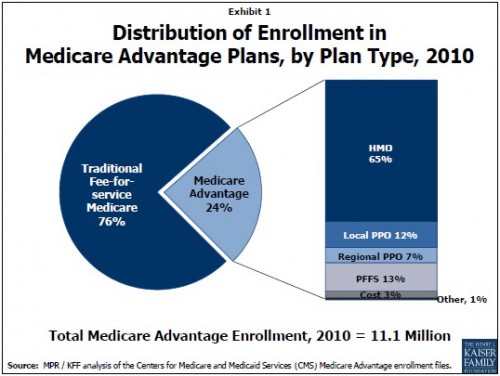
First, one thing I posted yesterday isn’t quite right. I wrote that “local and regional Medicare PPOs attract, respectively, only 8% and 3% of enrollment in all Medicare Advantage plans.” That was true last year, but this year the figures are 12% and 7%. So MA PPOs are growing. The following figure is from the Kaiser issue brief.
The second bit I learned from the issue brief is how the quality incentive payments will work.
Plans that receive 4 or more out of 5 stars from the health plan quality rankings will receive bonus payments of 1.5 percent in 2012, 3.0 percent in 2013, and 5.0 percent in 2014 and later years; high quality plans in certain counties will receive double bonuses.
The majority of plans will be allowed to retain only 50 percent of the difference between the plan bid and the benchmark, but plans receiving 3.5 or 4 stars will retain 65 percent of the difference and plans receiving 4.5 or 5 stars will retain 70 percent of the difference. Total payments to plans, including bonuses, will be capped at current payment levels.
OK! Now I know. By the way, don’t be confused by the use of the term “bid.” There is no competitive bidding going on because benchmarks are not a function of “bids.” I’m annoyed that the term “bid” is used because it hides the fact that this is administrative pricing. I’ll try to lighten up.