The Tuskegee Study was a longitudinal study of syphilis in which many participants died without receiving care for their illness. Study participants were black men. A new NBER paper by Marcella Alsan and Marianne Wanamaker argues that
the historical disclosure of the study in 1972 is correlated with increases in medical mistrust and mortality and decreases in both outpatient and inpatient physician interactions for older black men. Our estimates imply life expectancy at age 45 for black men fell by up to 1.4 years in response to the disclosure, accounting for approximately 35% of the 1980 life expectancy gap between black and white men.
Aslan and Wanamaker claim that the disclosure of the Tuskegee atrocity reduced older black men’s trust in the health care system. The growth in mistrust reduced these men’s use of health care. And the reduction in health care increased chronic disease mortality. I will summarize how they reach these conclusions and offer some reasons why we need to be cautious about believing them. These concerns parallel those raised by Aaron in the NYT. However, if the results are valid this is an important study and I will try to say why.
So, how does the study work? Alsan and Wanamaker use a difference-in-differences-in-differences design. They compare
black men before and after the Tuskegee disclosure (first difference), relative to a peer group of white men or black women (second difference) across an additional measure of cultural proximity to the study subjects (third difference).
That sentence went by fast, so let me spell it out. Alsan and Wanameker are not trying to explain the levels of black or white use of health care or mortality. Instead, this study is focused on a possible shift in the relative use of health care and relative death rates that began at a specific time (1972) and place (Tuskegee). That shift correlates with the time and place of the disclosure of the actrocity. From that correlation — and a correlation is all that it is — they infer that the disclosure was the likely cause of these shifts in health care use and mortality.
Now let’s look at the data. To get at attitudes toward the health care system, they used questions from the General Social Survey. In that survey,
participants were asked about whether “doctor’s judgment trusted” and whether “doctors deny me the treatment needed”.
Unfortunately, these questions were only asked in 1998, so we only know about attitudes toward the system after Tuskegee. But for that period, they found
that black men, compared to white men and black women exhibit a strong, statistically significant geographic gradient in both mistrust of doctors and concern regarding treatment denial. A one standard deviation increase in the proximity to Tuskegee, Alabama results in an increased probability of medical mistrust on the order of 9 percentage points compared to white men and 12 percentage points compared to black women.
For the use of health services, they found that
a one-standard deviation increase in geographic proximity to Tuskegee, Alabama reduced utilization of routine care (outpatient physician contacts) among older black males by 1.29 interactions per year when compared to their white peers and 0.97 interactions per year relative to black women, a 20-30% reduction in utilization relative to the pre-disclosure mean value for black men.
Finally, for mortality,
we find that a one standard deviation increase in geographic proximity to Tuskegee was associated with post-disclosure age-adjusted mortality increases among older black men of 3.5 log points compared to white men and 6.9 log points compared to black women.
Here are some of the mortality results:
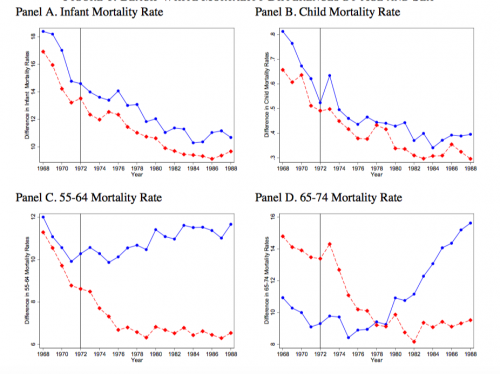
The vertical axis in each graph is the black-white difference in mortality and the horizontal axis is historical time. The blue lines are race differences for men and the red lines are for women. The different graphs are different segments of the age distribution. So, for infants and children (panels A and B) you see that black-white mortality differences decrease steadily over time. The same is true for older women in panels C and D. But for older men, black-white mortality differences rise after 1972.
We need to be cautious about accepting this story. As Aaron pointed out, this is a working paper, which means that it hasn’t been peer reviewed. Lots of smart people will chew through these results and it’s likely that they will raise questions. Many of these questions will focus on the correlational design. The Aslan and Wanamaker data suggest that something happened around 1972 somewhere in the American SouthEast. That could be the disclosure of the Tuskegee study, but it’s also possible that it was something else.
That’s not the only potential problem. Like Aaron, I am surprised that the effect appears only in men. Black women are well aware of Tuskegee. It’s hard to believe that the disclosure did not increase their mistrust of doctors or affect their care seeking.
But suppose that the authors’ story survives peer review. What does it mean?
It doesn’t mean that contemporary black-white differences in care seeking and mortality are primarily the result of the disclosure of Tuskegee. (Again, Aaron was right about this.) By design, the study looked at the effects of just one event, not the entire process shaping black-white differences in men’s attitudes toward the health system and care seeking. Those problems have many causes that have endured for hundreds of years. This paper describes one shock that occurred in Tuskegee in 1972 that coincided with increased disparities in service use and mortality for a subgroup of the black population. The finding that this shock had a major effect is entirely compatible with the view that enduring structural racism had a larger effect.
I think that the value of the study — if it stands up — is that it provides evidence of strong causal connections between trust in doctors, care seeking, and mortality.
First, it shows that trust in physicians varies across communities and is affected by those communities’ histories. In my experience, most health care providers have an unexamined assumption that people trust health care providers. Similarly, most health care institutions make only limited efforts to understand the cultures of the communities they serve. But if Aslan and Wanamaker are right, trust and legitimacy are more fragile than many assume. Moreover, their results suggest that care seeking is strongly dependent on trust. Understanding the cultural foundations of trust in doctor-patient relationships should become more than just an ancillary issue in medical research and training.
Second, if Aslan and Wanamaker are right, the decrease in care seeking by members of an impoverished group significantly harmed them. This finding deserves careful scrutiny in light of the continuing debate about the health benefits of increasing access to health care, for example through expanding health insurance coverage.

