This paper is going to really piss some people off. “Mortality and Treatment Patterns Among Patients Hospitalized With Acute Cardiovascular Conditions During Dates of National Cardiology Meetings“:
Importance: Thousands of physicians attend scientific meetings annually. Although hospital physician staffing and composition may be affected by meetings, patient outcomes and treatment patterns during meeting dates are unknown.
Objective: To analyze mortality and treatment differences among patients admitted with acute cardiovascular conditions during dates of national cardiology meetings compared with nonmeeting dates.
Design, Setting, and Participants: Retrospective analysis of 30-day mortality among Medicare beneficiaries hospitalized with acute myocardial infarction (AMI), heart failure, or cardiac arrest from 2002 through 2011 during dates of 2 national cardiology meetings compared with identical nonmeeting days in the 3 weeks before and after conferences (AMI, 8570 hospitalizations during 82 meeting days and 57 471 during 492 nonmeeting days; heart failure, 19 282 during meeting days and 11 4591 during nonmeeting days; cardiac arrest, 1564 during meeting days and 9580 during nonmeeting days). Multivariable analyses were conducted separately for major teaching hospitals and nonteaching hospitals and for low- and high-risk patients. Differences in treatment utilization were assessed.
Exposures: Hospitalization during cardiology meeting dates.
Main Outcomes and Measures: Thirty-day mortality, procedure rates, charges, length of stay.
So here’s the gist. There are two big cardiology meeting every year, and when they occur, lots of cardiologists go to them. Fewer of them are left home to care for patients. So the researchers looked at how patients admitted to the hospital fared during those meeting dates compared to the three weeks before and after the conferences. Specifically, they looked at 30-day mortality for patients admitted with acute MIs, heart failure, or cardiac arrest.
When I first looked at this, I assumed that they were concerned that patients would fare worse during the meetings. I thought they were worried with all the cardiologists off at meetings, patients might have worse outcomes.
The opposite happened.
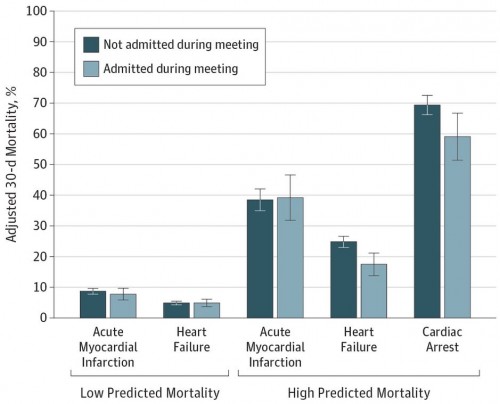
High risk patients admitted with heart failure during meetings had a 30-day mortality rate of 17.5%, compared to 24.8% when more cardiologists were there. Cardiac arrest 30-day mortality was 59% during meetings and 69.4% at other times. Not surprisingly, the rates of percutaneous coronary intervention were lower during meetings, too (20.8% versus 28.2%).
So obviously, there are some top level concerns here, and the researchers addressed some of them. Maybe any meeting affects patient care. But they found that cardiac mortality wasn’t affected by oncology, gastroenterology, or orthopedic meetings. They also found that mortality from GI or orthopedic issues wasn’t affected by hospitalization during the cardiology meetings. This was strictly a cardiology meeting associated with cardiologic outcomes.
They have no measurement of staffing during those meetings, so we can’t really know what was the cause of the finding. Were fewer cardiologists really available?
There are a number of ways to interpret this. Maybe the best cardiologists were the ones who stayed home. Maybe with fewer cardiologists available, fewer invasive procedures get done, and that leads to better outcomes. Maybe they tell more low-risk patients to wait when fewer cardiologists are available, which gets the higher risk patients more attention and better outcomes. Maybe it’s something else.
But here’s the thing. Whatever is different during the meetings, it’s associated with lower intensity care and better outcomes. That’s probably worth looking into.