From Health Affairs, “State Spending On Dual Eligibles Under Age 65 Shows Variations, Evidence Of Cost Shifting From Medicaid To Medicare“:
Roughly half of Medicare beneficiaries under age sixty-five are also eligible for Medicaid. These “dual eligibles” have been the subject of much research because of their low income and poor health status. Previous studies suggest that some states seek to shift costly health care services for this group out of state-run Medicaid programs and into the federally funded Medicare program—for example, replacing nursing home care with hospital care. Using state-level data on dual eligibles under age sixty-five, we found support for this hypothesis. In states with below-average per capita Medicaid spending, corresponding Medicare spending was above average. These state-level estimates also revealed a nearly threefold difference in total—Medicare plus Medicaid—price-adjusted spending per person, ranging from $16,309 in Georgia to $43,587 in New York. Such large variations among people with serious diseases suggest inefficiency. Some states may be spending too little for Medicaid, meaning that some patients’ needs are not being met, or some states may be spending too much, meaning that more services are being provided than needed. Such inefficiency exposes patients to unnecessary risk, drives costs up unnecessarily, and highlights the large potential gains arising from improved care coordination for dual eligibles.
Can we start with the fact that half of people over 65 can qualify for Medicaid? That speaks pretty poorly about the financial stability of the elderly population. (ed – Sorry – I’m tired and I misread. This is besides the point anyway so ignore – Aaron)
Once you get past that, though, this manuscript speaks pretty well to the potential pitfalls of keeping Medicare and Medicaid financed at different levels of government. Medicare, of course, is a federally run single-payer system for everyone over 65. Medicaid, on the other hand, is a state run system where the federal government matches some percentage of payments so that states aren’t totally responsible for financing. The trick, though, lies in the dual eligibles, or people who are on both Medicare and Medicaid.
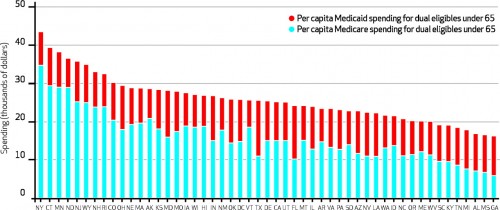
States, of course, would like the federal government to pay for more so that they can pay for less. So whatever they can get shifted to Medicare for dual-eligibles, the better. Medicaid, for instance, pays for nursing home care (which Medicare does not), so if they can get a patient admitted to the hospital instead, then they can get Medicare to pay. But this probably isn’t good for patients. If that was occurring differently in different states, you’d expect great variation in the amounts states spend on Medicaid versus Medicare:
If people are unhealthy, you’d expect more health care spending period. But as you can see, the proportion spent on Medicare versus Medicaid is all over the map. This means that states are likely finding ways to get Medicare to pay for a larger percentage of care in some states. Here’s a better way of looking at that:
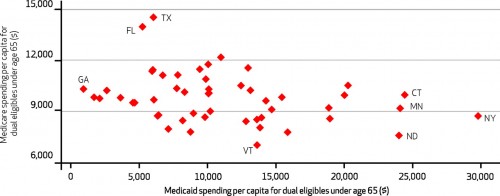
There’s really no positive relationship between Medicare spending per person (x-axis) and Medicaid spending per person (y-axis). You’d expect that if increased spending was just a measurement of “illness” in the population. There is, however, a negative relationship:
We also found evidence of a negative association between Medicaid and Medicare spending for dual eligibles under sixty-five (Exhibit 3), with a weighted correlation coefficient between Medicare and Medicaid spending for this group of −0.40 (
). That is, for these beneficiaries, Medicare expenditures appeared to substitute for Medicaid expenditures. States with lower rates of Medicaid spending experienced higher rates of Medicare expenditures, and vice versa.